Proceedings of the Subcommittee to
Update "Of Life and Death"
Issue 4 - Evidence
OTTAWA, Monday, February 28, 2000
The Subcommittee to Update "Of Life and Death" of the Standing Senate Committee on Social Affairs, Science and Technology met this day at 1:03 p.m. to examine the developments since the tabling in June 1995 of the final report of the Special Senate Committee on Euthanasia and Assisted Suicide, entitled, "Of Life and Death".
Senator Sharon Carstairs (Chairman) in the Chair.
[English]
The Chairman: Good afternoon, everyone. Today is our fourth hearing under our mandate to update the unanimous recommendations of the 1995 Special Senate Committee report on euthanasia and assisted suicide entitled "Of Life and Death." I would remind everyone -- honourable senators, witnesses, and those watching on television -- that this committee is not reopening its debate on assisted suicide and euthanasia; it is dealing strictly with the areas of the report where the original committee made unanimous recommendations. I would ask that everyone bear that in mind as we proceed with the hearings.
Before us today are three panels of witnesses who have been invited to address us on the issues that were raised in the report for which there were unanimous conclusions. First, we have the officials from Health Canada. Later this afternoon we will hear from representatives of the Elisabeth Bruyère Health Centre. Our third panel will consist of Professor Peter Singer from the University of Toronto and Professor Harvey Chochinov from the Department of Psychiatry, University of Manitoba.
We will begin with the witnesses from the Department of Health and Ms Barbara Ouellet, Director of Home Care and Pharmaceuticals. We would ask all the witnesses to be as short and as succinct as they possibly can because the senators gathered will want to ask them many questions.
Please proceed.
Ms Barbara Ouellet, Director of Home Care and Pharmaceuticals, Health Care Directorate, Policy and Consultation Branch, Department of Health Canada: We have relatively brief remarks to make to you today. We will make our remarks first and then collectively entertain your questions. My remarks today will focus on the work we are doing in the area of home and community care, which includes palliative care as one of the aspects of treatment of clients in that area.
It is a pleasure for me to be here today to update you on our work and to speak a bit about how our work relates to the Senate report "Of Life and Death" that was tabled in June of 1995. Following the tabling of the report, Health Canada established an inter-branch committee to review the recommendations and to assess how action in these areas might be incorporated into the work of the department. In fact, we have discovered that the completed and ongoing work of the department touches directly or indirectly on many of the committee's recommendations relating to palliative care. I and my colleagues here today will be updating you on some of these initiatives. I would also mention that we have already begun to prepare a summary of the relevant work that we have been doing to date. Once this work is completed, I would be happy to provide that to the committee members for your information.
One of the key recommendations of the Senate report was that governments make palliative care a top priority in the restructuring of the health care system. In September of 1998, all health ministers identified continuing care, which encompasses home and community care and institutionlized long-term care, as one of their key priorities for collaborative action. In September, 1999, health ministers reviewed progress to date and reaffirmed their commitment to these priorities.
In follow up, officials within the department have been working with our counterparts in provincial and territorial health ministries to assess the major pressures and changes facing home and community care, and to identify possible directions and priorities for enhancing services in this sector. In addition, our focus is on how to strengthen the coordination and linkages within other sectors of the health system and between these sectors -- for example, between home and community care and primary, acute and long-term care -- in order to ensure that Canadians have more seamless access to an integrated array of services based on their health needs.
In particular, we are in the process of preparing a detailed overview of current home and community care programs, including the range of available services, client entitlements and current budgets. We have also begun to consider possible common objectives that all jurisdictions could agree on and which would set a realistic but progressive vision for strengthening home and community care over the near and longer term.
Palliative care is one of the types of client needs that is usually addressed through home and community care programs. In this sense, then, our focus is on integration within and across the sectors of the system and, in doing so, will be consistent with the recommendations of the Senate report that spoke of this need in regard to palliative care.
One of the other recommendations of the report concerned promoting and supporting research into palliative care. The subcommittee may be interested to know that home care is one of four priorities under the Health Transition Fund. This fund was announced in the 1997 budget and totals $150 million over about three to four years. In addition to home care, other priorities of the fund include primary care, pharmaceuticals, and integrated service delivery.
A number of projects in the areas of home care and integrated service delivery focus on palliative care. For example, one project which is supported by both the Nova Scotia and Prince Edward Island Ministries of Health is a demonstration project on rural palliative care. We have a project in Quebec which is supported by one of the CLSCs that is looking at the development of an information and training guide on home care and services for persons with cancer. Another CLSC is leading a project looking at the development of a continuum of care and services for ill adults. Finally, a project in Saskatchewan is reviewing and evaluating the current palliative care program in one of its health districts.
In summary, then, as I believe I have indicated, there is already quite a bit of work that is underway and that will be continuing with respect to palliative care. In view of the agreement among FPT ministers to give priority attention to home and community care, this will be an area of ongoing collaborative work aimed at strengthening the availability and integration of such services, including those related to palliative care.
Ms Nancy Garrard, Director, Division of Aging and Seniors, Health Promotion and Programs Branch, Department of Health Canada: I am also pleased to be with you today to discuss this important issue.
The role of the branch on this issue is varied and includes support for community-based initiatives, public and professional education, knowledge development and dissemination, as well as collaboration between governments and agencies on various shared projects. The branch focuses on addressing health issues across the lifespan using a population health approach.
By using this approach, Health Canada recognizes the importance of end-of-life issues across the entire spectrum of life stages: childhood and youth, mid-life and later life. We certainly see a particular need for attention for end-of-life care issues for Canadian seniors. As you probably know, over 75 per cent of all deaths in Canada occur in people over the age of 65. Certainly, with the aging of Canada's baby boom generation in the coming decades, end-of-life care issues, including palliative care, will become even more prominent.
Under the "Promotion of Population Health" business line adopted in 1997 by our department, addressing end-of-life issues is noted as one of the four priority themes for the later life population. This priority has continued over the past three years and was selected partly as a result of the findings and recommendations of the Special Senate Committee report, "Of Life and Death."
The majority of our work has been in supporting innovative community projects to raise awareness of end-of-life concerns amongst the health community and other stakeholders. We have also supported the development of public education materials, knowledge dissemination activities and support for national health voluntary organizations working in this field. In total, we have contributed over $2.9 million over the past five years to these initiatives. In particular, we have funded 10 major community initiatives pertaining directly to end-of-life issues for seniors as well as six major projects pertaining to the care of HIV/AIDS patients. These particular projects have been consistent with many of the recommendations made by the Special Senate Committee.
One example is the development of a manual of national guidelines to support the end-of-life care of seniors. This project is sponsored by the Sunnybrook Health Science Centre at the University of Toronto. The guidelines, which are consistent with the recommendation of the development and implementation of national guidelines, are scheduled to be released this spring.
Another example is the support we provide to an international symposium on care of the dying. This is a project sponsored by the Sisters of Charity of Ottawa Health Services. The symposium will take place in April, 2000. This is consistent with your recommendation that research into palliative care be expanded and improved and disseminated to those who need this information.
We have also developed a 17-module national palliative care training package for health support workers and the implementation of a national network of educators to deliver this training program. The multiyear project will be in conjunction with the Canadian Palliative Care Association as well as the Canadian Association for Continuing Care. This is consistent with your recommendation that the training of health care professionals, in all aspects of palliative care, be increased. To date, this package has been well received and used by the health care community.
The branch has also facilitated the dissemination of information to the general public through the publication of a palliative care information sheet for seniors. I have made a copy of this available to the clerk. This was a joint project with the provinces and territories under the auspices of the federal, provincial and territorial ministers responsible for seniors. Health Canada also sponsored the Invitational Symposium on Palliative Care: Provincial and Territorial Trends and Issues in Community-Based Programming in March 1997, in Ottawa. The report from this invitational symposium is available on the Health Canada Web site, "Division of Aging and Seniors."
We have supported community development for palliative care under the HIV/AIDS programming. We have also supported some developmental work on hospice palliative care that has been started by the Canadian Palliative Care Association. Between 1995 and today we have provided $338,000 to the Canadian Palliative Care Association, a major national voluntary health organization, for their development, operating costs, strengthening their governing structure and the volunteer leadership base that is important to develop community capacity across Canada.
End-of-life and palliative care issues are also on the agenda of other health care stakeholders' organizations. For example, the National Advisory Council on Aging, which is an order-in-council body, devoted its spring 1998 issue of its newsletter, Expression, to issues related to seniors and palliative care. I have also left copies of that for your subcommittee. NACA, as it is usually called, also identified palliative care as a major challenges in its recent publication, 1999 and Beyond: Challenges of an Aging Canadian Society.
In conclusion, we believe that dealing with end-of-life issues is important to ensure that Canadians have a comprehensive health system that provides support throughout a person's life. In the years ahead, we anticipate continuing to develop and disseminate knowledge about palliative care and other end-of-life issues, and we will certainly be working to help develop community capacity in this area.
Dr. Christina Mills, Director, Cancer Bureau, Laboratory Centre for Disease Control, Health Protection Branch, Department of Health Canada: The cancer bureau has a mandate to develop evidence relevant to a broad range of cancer control activities from primary prevention right through to palliative care. We aim to create the evidence where it is missing, strengthen it where it needs that, and to facilitate the use of information, real evidence, for the planning and development of policies and programs.
Palliative care is just one of six components of cancer control, but it is considered a key component. It supports the aim of improving quality of life for cancer patients at the end of their lives. Cancer patients account for the vast majority of palliative care patients.
With the aging of the baby boom population, we know that, even if rates of cancer stay substantially the same as they are now, the number of cancer patients and, hence, the number of palliative care patients in the future will greatly increase. This trend is indicated in the notes that I provided to the Clerk.
It is commonly reported that only about 5 per cent of dying cancer patients have access to palliative care. We do know that the situation has improved somewhat in some jurisdictions since those early studies, but the fact is that we do not know enough about what is going on across the country. We are aware of important geographic variations, but there has been no systematic means of determining exactly what is happening in respect of palliative care across Canada.
The activities of our bureau relate to your recommendations to strengthen research in palliative care and to sponsor a national information program. We are bringing our grain of sand to what, we hope, will be a national information program.
The surveillance information, if it were available, would indirectly contribute to responding to your recommendations concerning national guidelines and standards, the training of health professionals, as well as the recommendation that there be an integrated approach to palliative care.
Since the original report containing the recommendations, we have co-sponsored and contributed to a number of national meetings that relate to palliative care surveillance issues. Many of these meetings dealt with precisely the issue of standards and common definitions of terms for surveillance. We have contracted with researchers to conduct studies and develop methods for the surveillance of palliative and end-of-life care.
We sponsored a pilot project to study the feasibility of collecting needed information to monitor palliative care in Canada. Six palliative care centres or programs in five cities across the country have volunteered to supply data from their program databases so that we can assess the data and determine the extent to which that would serve as the basis for systematic monitoring.
Through our Canadian Childhood Cancer Surveillance and Control Program, we have conducted a survey of parents regarding their access to supportive care and the types of supportive care provided to their children prior to death. The results of this are not available as yet.
Through our partnerships with the Canadian Coalition on Cancer Surveillance and the Canadian Strategy for Cancer Control, we have identified palliative care as one of the key components that needs to be addressed in both those efforts.
The pilot projects taught us that cancer patients accounted for more than 90 per cent of those receiving palliative care. Nearly all of these had metastatic disease. The distribution of cancer sites was comparable to the distribution of the main forms of cancer deaths.
We learned that the programs are moving towards the goal of better integration of institutional and home care. Previous speakers alluded to that goal. We hope this will enable patients to be assigned to the level of service most appropriate to their particular needs to ensure the best quality of life. Because the services are provided in such a broad range of settings, this provides a real challenge to collecting consistent and comparable information across different sites.
Programs may be partially integrated across services or may sometimes operate as parallel structures. One element that has already been demonstrated in a small way is that reducing the demand for expensive acute care hospital beds is a beneficial side effect of having these programs in place.
Through the pilot studies, we also identified an array of information needs. It seems that every time you start to collect information, you principally find out that you need more. The information is needed to plan and monitor programs and to improve our knowledge about how palliative care can most effectively be delivered. There is no information system in place, or even a combination of systems, to collect population-based data on palliative care at the national level. A few health regions may be able to provide a relatively complete picture, but there are gaps even in the best-developed systems.
We need information to follow trends in the use of services, to monitor development of new services, to assess the effectiveness of services in relation to models of service delivery, and to help plan for future services and resource delivery.
Any development of information systems will need to take into account the diverse settings in which palliative care is delivered, the local and regional nature of palliative care program development, as well as the diseases other than cancer that contribute to palliative care. As you know, AIDS and dementia are contributors to palliative care.
We need consistent and consensus-based definitions for data collection and standards of data to be able to provide information that is comparable across the country. In my brief I have outlined a couple of possibilities concerning how we can build on this. The two approaches are "incrementally", as we have been attempting to do, and "strategically", to identify where we most need the resources and to build capacity. I will not go into more detail about those.
Planning programs and developing policies in the absence of the relevant and appropriate surveillance information, compared to doing the same thing with the relevant and appropriate information, is the difference between taking aim at a target of known size and location and playing pin the tail on the donkey. In palliative care, we cannot afford to be playing pin the tail on the donkey.
Ms Debra Gillis, Director, Health Programs Support Division, Medical Services Branch, Department of Health Canada: Thank you for the opportunity to address the committee. The Medical Services Branch of Health Canada is the branch that holds responsibility for the delivery of health services to First Nations and Inuit.
Today I will provide the committee with information on steps that have been taken to address aboriginal issues raised in "Of Life and Death," that, in particular, are related to palliative care.
By way of background information, there are approximately 630,000 First Nations people and 45,000 Inuit people in Canada today. Just over half of First Nations people live on-reserve. As many of you know, health issues are of particular concern to First Nations and Inuit who experience rates of communicable and chronic disease significantly greater than those in the general population. Conditions which have become more prevalent over the past decade include diabetes, cancers, HIV/AIDS and cardiovascular disease.
While total mortality rates are similar to those of Canada as a whole, there are some exceptions. For example, infant mortality is twice as high. Death from suicide for youth is five to eight times greater amongst the First Nations population. Issues related to life and death are very significant for First Nations for a number of reasons.
The Health Canada mandate for health services delivery is directed specifically to First Nations and Inuit. All First Nations and Inuit, whether they live on-reserve or not, receive hospital and physician services through the provincial and territorial insured health services. Aboriginal people living off reserves access community-based health services, such as public health and home care, through the provincial and territorial health systems.
Health Canada, and Medical Services Branch in particular, is responsible for the delivery of community-based health services on-reserve, as well as non-insured health benefits, including prescribed pharmaceuticals and medical supplies and equipment to all First Nations and Inuit. The lack of availability of palliative care services for aboriginal people has been identified as a critical issue.
I am pleased to inform the subcommittee that Health Canada is taking significant strides to address this issue on reserve. In the February 1999 budget, funding was announced for the development and implementation of a home and community care program on-reserve and in Inuit communities. Prior to that time, home care services had been limited to homemaking support through the Department of Indian Affairs and Northern Development and very limited home nursing provided by Health Canada. With the introduction of this new program at $90 million per year beginning in 2002-03, First Nations and Inuit will be able to provide the full range of home care services now available to other Canadians.
While there is not a specific palliative care component in this program, the home nursing, personal care and in-home respite components of the program will go a long way to supporting individuals and their families who choose dying at home and palliative care as an option. Discussions have begun with First Nations, as they develop the home and community care programs, on how palliative care needs can be incorporated into their program.
Off reserve, First Nations and Inuit have access to palliative care programs provided through provincial and territorial health services where they exist. First Nations and the Inuit have identified that these programs need to incorporate more traditional aboriginal approaches to dying for their members and, where possible, are working with programs to do so.
Medical Services Branch also supports palliative care through its non-insured health benefits program. This program, available to all First Nations and Inuit, without restriction of residency and income, covers a wide variety of drugs used in the management of pain, including narcotic agents which are available in a variety of dosage forms, including oral and injectable forms. The narcotic drugs, as with all pharmaceuticals under this program, must be prescribed by a physician and must meet federal, provincial, and territorial laws and regulations. Thus, access to the wide variety of pharmaceuticals used in palliative care is unrestricted for First Nations and Inuit, given that they are prescribed by their attending physician.
Health Services Branch has also begun to address the palliative care needs of aboriginal people with HIV/AIDS and their caregivers. There are many instances where aboriginal AIDS patients wish to return to their home communities during the end stages of this condition. To assist the family and other caregivers, including health professionals, we have funded, in conjunction with the health program and promotion branch, the Two-Spirited People of the First Nations to produce Nashine Ginwenimawaziwin -- Constant Care, a manual on palliative care for aboriginal communities. This publication is widely available and used.
In closing, Health Services Branch has taken some steps to enhance access to palliative care services for First Nations on-reserve and for Inuit. I would be pleased at a later time to answer any questions you may have.
Mr. Cliff Halliwell, Director General, Applied Research and Analysis Directorate, Information, Analysis and Connectivity Branch, Department of Health Canada: Honourable senators, the Applied Research and Analysis Directorate is a new directorate within Health Canada. Its role is to support quantitative analysis, especially economic analysis, in support of both policy decision making and accountability for Health Canada's programs and activities.
Although the directorate was created in November 1998, staffing only began in the spring of 1999, and is still underway. Some research activities are now underway, mostly related to aging, health human resource issues, and health system renewal in general.
One element of the directorate existed prior to its formation, the National Health Research Development Program, NHRDP as it is known. This is a program to fund investigator-driven health research in Canada, as well as supporting young researchers through a personnel awards program.
While requests for funding to NHRDP are largely investigator-driven, Health Canada does indicate to researchers the areas in which it would like to see research done and where it would be most supportive of the research activities. To be successful, proposals must go through a rigorous peer-review process to ensure quality.
Since the 1995 committee report, NHRDP requests for proposals have included requests for research on end-of-life and palliative care issues. Some of the most useful forms of research the NHRDP funds are synthesis projects. These projects provide a summary of the state of knowledge in particular areas.
In 1997, the NHRDP released a request for proposals for synthesis projects that included projects on end-of-life and home care. The end-of-life section quoted the Senate Special Committee on Euthanasia and Assisted Suicide's recommendation that research be undertaken into how many individuals are requesting assisted suicide, why it is being requested, and whether there are any alternatives that might be acceptable to those who are making the requests.
This section of the RFP outlined two scopes of synthesis projects required. The first was synthesis of research and evidence on factors affecting the desire of terminally ill or seriously chronically ill persons to hasten death. The second was synthesis of research and evidence on chronic pain management.
The home care section focused upon providing support to informal caregivers. Again, there were two projects set out. The first was synthesis of research evidence on the effect of formal palliative care services on family caregivers' physical and mental health and well-being. The second was synthesis of research and evidence on the effects of financial compensation or payment on each of caregivers and care recipients as compared to other supports, such as community services. In total, for those two competitions, five projects were successful.
In addition, three other synthesis projects relating to the recommendations of the committee have been funded in the last three years.
As well, NHRDP has annual general competitions to look at specific research proposals in specific areas. Since 1995, the NHRDP has funded nine such projects which address the committee's recommendations. These nine do not include the most recent competition for which research proposals are still under review.
As well, through its personnel awards, the NHRDP has funded at least two researchers who have conducted work on palliative care and pain management.
In total, since 1997, NHRDP has funded around $1.2 million worth of research and personnel awards relating to these issues. We will prepare for the committee a list of the related projects. Committee members will be free to request either the summaries or, indeed, the full studies.
To give you an idea of what kinds of studies these are, the first two synthesis projects that were funded included: "The Desire to Die or to Hasten Death in Terminal Illness: A Literature Synthesis," produced by Queen's University; and "Synthesis of Research and Evidence of Factors Affecting the Desire of Terminally Ill or Seriously Chronically Ill Persons to Hasten Death," which is out of the Université du Québec à Montréal.
In addition, the NHRDP is working to mobilize the research communities to the issues of palliative care. In its requests for 1999 annual general competition proposals, we solicited letters of intent in areas addressing issues including aging, home care and financing of the health care system.
The requests for proposals specifically called for projects addressing the integration of palliative care with long-term care. Through this competition, at least 11 research proposals were received addressing issues of end-of-life care, euthanasia, physician-assisted suicide and palliative care. These proposals are still currently under peer review and it will be some time before results are available.
The Chairman: You have given us a great deal of information. We heard in our first three presentations that little progress had been made. It is rather reassuring to hear that the Department of Health people have put their minds to the Special Senate Committee report. It is particularly good to hear that it has been used to describe certain situations on occasion. It is also fair to say that your comment that there is still a long way to go is reflective of the testimony we have heard during our other three days of meetings.
Senator Beaudoin: We are all in favour of palliative care. Who is against it? That was the feeling of the committee members in 1995. We have made some progress but we must act immediately to improve the situation. What must we do immediately in the area of palliative care? The report is now five years old. Must we legislate? Must we consult the provinces or do more? What must we do to update the report on palliative care? I have taken notice of everything you said and many things have been accomplished, but what else needs to be done?
Mr. Halliwell: Clearly, as Dr. Mills has said, better information would be helpful. We do not yet have a good sense of whether the issues that arise when these cases make headlines quite often arise when dealing with dying patients, or whether they rarely arise. The guidelines that are in place in the medical community handle quite a few of the cases that could arise.
Of course, we have just heard how difficult it is to acquire this information. It is especially difficult because these would be very sensitive questions. There is no doubt that the first step would be to try to acquire further information through pilot projects, such as those that have been described, to get a sense of the extent of the problem.
After that, I must say that this is an extraordinarily sensitive subject that touches very much upon Canadians' values. There are tremendous moral and ethical issues involved that must be dealt with at what is one of the most difficult times in a person's life, namely, when the person is dealing with the impending loss of a loved one.
I am not sure to what extent research can lead us to a better articulation of the values that should be used in making these decisions. It is something that must come out of a process that finds out what Canadians' values are in this area and tries to achieve consensus. I do not think it is an activity that lends itself to a simple approach of research or, in particular, data gathering. That would be useful, but it would not answer the questions.
Senator Beaudoin: Have you considered the possibility of enacting new legislation in the field of palliative care? Having regard to the fact that part of this problem is provincial, as well as federal, have you had meetings with your counterparts in the various provinces?
You refer, I believe, to Quebec plans and others, and Dr. Gillis referred to the aboriginal people. My impression is that we must legislate in this area, and that we must include the provinces in any discussions. Since there is unanimity on the need for palliative care, and since the provinces and the federal authority have much to do, do you think that we should legislate? I think we should.
The other day Dr. Brazeau told us that we do not need to amend the Criminal Code. I was somewhat surprised that he made that comment, but his is a point of view for which I have the greatest respect. What do you think about that particular subject?
Ms Ouellet: Since I am the one who often has discussions with provinces on these matters, perhaps I can answer that.
We have considered, with the provinces, the issue of palliative care. In fact, one of the items that will be provided to you is a report that we produced in 1997 which was an overview of provincial and territorial palliative care programs.
The problems facing palliative care are, in many ways, synonymous with the problems provinces now face in trying to provide adequate home and community-based services for a whole array of community needs. The reality is that, within our health care system, we have taken great measures to better organize and restructure and, in some cases, even downsize our acute care system. However, we have not yet seen corresponding developments within the community and within a home setting to enable us to ensure that those people's needs will be adequately met.
I suspect -- although I do not have the data on this and perhaps my colleague, Nancy Garrard, does -- many people with a terminal illness who are in hospital would want to choose the option of dying at home, in their community, if the proper supports were available, as opposed to remaining in a hospital. We must continue to address the questions: What needs are we effectively meeting in the community in terms of care at this point; and what needs are we not meeting? From my discussions with provinces it is evident that there is considerable variability across the country in terms of what home and community care services are currently available. In almost every province those services are under stress, as we see the downsizing from the acute care sector and, at the same time, a desire not to overly increase the institutionlized long-term care sector.
I am not sure that legislation is necessarily the issue. I think we must look at our system in a much more integrated way and consider how, perhaps, pressures and challenges in one part of the system are inadvertently -- or because of a delay in other initiatives -- being off-loaded onto other parts of the system that are not yet able to meet those needs.
Ms Gillis: With aboriginal people, there are two issues. One is the relationship to the new home and community care program that is being developed by aboriginal people, First Nations and Inuit. This is a major stride forward in palliative care, but it is too early to know what the issues are and how well that program will address some of the palliative care needs.
The intent of the program is full maturity within another two to three years. How communities go about addressing those needs will vary across the country. It is a little too early to know whether or not this program is addressing the palliative care needs of those living on-reserve. I think it is taking us a long way forward. Within the next four to five years, we will have a good idea of what is in place and how it is addressing the palliative care needs; what is and is not being met through this program; and then what needs to be put in place to do so.
The other issue for aboriginal people who do not live on-reserve are the same issues that Ms Ouellet mentioned, because they access the provincial health system. The strains on the provincial and territorial health system, in many ways, are reflected in the ability of aboriginal people to access palliative care services in the community. That is further enhanced by services within the provincial system that are often not culturally sensitive, as First Nations and Inuit and other aboriginal people have pointed out. That is being worked on. However, I know of instances and I have been told of instances where hospitals are becoming much more sensitive to the needs of dying patients, of bringing traditional healers and elders into the hospital, of families being there when a person is dying, as they would in the community. Hospitals are becoming much more open to the culture and traditions of aboriginal people. That is a step forward. There is a long way to go but, I think, bit by bit, things are happening.
Senator Beaudoin: How many times a year do Ministers of Health meet, or how often do the officials, such as the deputy minister or assistant deputy minister or directors meet? There must be many meetings a year.
Ms Ouellet: Yes, there are. There are meetings at all levels including at the level of ministers and deputy ministers. There are also four senior policy advisory committees that report through that structure and they comprise a whole array of groups. In almost any given month I think it is safe to say there will be numerous federal-provincial meetings, and in between that there are many conference calls.
Dr. Mills: I wish to address the senator's previous question. Speaking as a public health physician I can say that a fairly systematic code of ethics has been developed for determining what interventions, from the public health perspective, are valid and appropriate. We look at the range of options available, including legislation, regulation, education, provision of information, and so on, and we choose the least intrusive means which will achieve the desired effect.
We know that information can be a tremendous driver for change. The Canadian Council on Health Services Accreditation now includes documentation of symptom control as part of its criteria for accreditation of health facilities. We expect that, in itself, will have an important clinical impact on patient care at the end of life because, in order to get accreditation points the health facility will have to document whether the patient was in pain, throwing up, et cetera.
In terms of the bigger system, you can draw an analogy from that situation in terms of surveillance of access to palliative care. Recently, people have been saying that 5 per cent of Canadians have access to palliative care. That may be true in some provinces but not in others. If we had good information on the actual levels of access to palliative care across the country, that would be an important driver for provinces with low levels of access to implement policies and programs which would improve access for their own citizens. If they did not take that initiative on their own, the citizens would soon make them think about doing it.
[Translation]
Senator Corbin: It would have been useful to have some information on the overall organization of the Department of Health, specifically with respect to health care, research, et cetera. I have observed that there are spokespersons from five different branches of the department. Should I presume that the department has other branches? Honestly, this is a bureaucratic jungle. I do not know which way to turn when there is talk about the Department of Health. Does the department have a director? Obviously, the minister, the deputy minister and the assistant deputy ministers are part of the department. However, can anyone answer this question: is there a palliative care coordinator at the Department of Health who gets all these people together on a regular basis to develop priorities, to coordinate activities in all the various fields, and to provide analysis and update us on any new developments about our sector of interest at this time? I appreciate the information you provided, but I will have to reread it and analyze your different perspectives to get a general idea.
[English]
Ms Ouellet: As I indicated in my opening remarks, following the release of the 1995 report, Health Canada established an interbranch committee specifically focused on reviewing and considering the recommendations from the committee's report. It looked at how our existing work within the department, which covers five branches, was already fashioned in a way that it supported these recommendations and at what other initiatives we have taken. I did not chair that interbranch committee, but the inventory of our activities, which I have offered to provide to you, is the result of much coordination and collaborative work across the department that has been undertaken since that time.
The fact that we have five witnesses here today in many ways speaks to the importance we place on the issue of palliative care and that we are trying to address it throughout the department. I believe that it is a strength rather than a weakness that five branches are actively studying this.
However, we do have an interbranch committee and we stay in touch with each other on a regular basis so that we know what progress we are making, both individually and collectively.
[Translation]
Senator Corbin: Have you run into federal-provincial jurisdiction problems in implementing your different programs, whether it be with the administration of services, analysis, information services? How much co-operation, or lack of co-operation, if that is the case, do you receive in your effort to establish a national palliative care system? Is this a problem?
[English]
Ms Ouellet: I will answer that question from the point of view of health care services, and then perhaps Mr. Halliwell would like to add something on the research side.
As one of the policy advisory committees that I mentioned to you, we have a federal-provincial policy advisory committee on health issues. This committee is concerned with the whole array of services, whether that be in hospitals, in the community, primary care, or other services. This committee meets regularly and has a very proactive agenda, including issues with respect to continuing care and home care, where a good deal of palliative care also takes place.
For the last many years I have chaired the federal-provincial working group on continuing care. My office is currently involved in some discussions with provinces on home and community care. The cooperation and dialogue are very good. All provinces and territories, which have the primary responsibility for delivery of services, rather than the federal government, are interested in learning from each other with regard to what they are able to do with their available resources, what models of delivery of service seem to work well, and what else we can learn about challenges and pressures that one jurisdiction has already addressed and another jurisdiction would like more information on.
There is a high degree of interest in good learning exchanges between jurisdictions. All jurisdictions know that home and community care is the sector which they are most pressed to grapple with as our population ages and as we undertake other changes within the health system that more and more promote care in the community. All this work has been reinforced by the commitment and by the agreement of ministers of health to make home, community care and continuing care part of their priorities. I mentioned that they initially agreed upon this in 1998. They reinforced it as a definite priority for collaborative work, as well as work within their own jurisdictions, when they met in September 1999.
Therefore, the cooperation is there. Individual jurisdictions face their own unique challenges, challenges that the jurisdictions themselves will certainly need to address. There is much that we are already learning from each other. There is also a good platform on which some collaborative work is being undertaken.
[Translation]
Mr. Halliwell: In the research, and more specifically, in the information services, there is a climate of co-operation. All of the projects funded by Health Canada are in the public domain, and therefore can be consulted by anyone who wishes to do so. We might be able to do a better job when it comes to publicizing our work. This information is available to all the provincial authorities.
In the research field specifically, it may be possible that the provincial departments, because of budget cutbacks, are limiting their study of research projects undertaken in the communities, specifically those undertaken by university researchers. This problem should be fixed now.
The Canadian Health Services Research Foundation is doing a lot of work to facilitate the exchange of information between researchers and governments. The Foundation demonstrated that this service was under-utilized once the research projects had been given a go ahead. Most of the information comes from three main sources: Statistics Canada, Health Information Services of CISTI and administrative databases, mostly provincial. There has always been a tradition to share this information when it is possible, however we have to respect the confidentiality principle, especially given the field of health.
However, it is not easy simply exchanging information with other researchers. For example, many of Statistics Canada's detailed databases are not readily available at Health Canada.
Senator Corbin: That is an important issue, and you should have access to this information to complete your research. How do you get around these problems?
[English]
Ms Leslie Gaudette, Section Head, Treatment and Palliation Section, Cancer Control Assessment and Surveillance Division, Cancer Bureau, Laboratory Centre for Disease Control, Department of Health Canada: We recently met with representatives of our palliative care centres. As a result, there are two points I wish to make. The first has to do with the level of the organization of the services and the effect of that on our ability to measure it. The second has to do with some of the databases, and so on, that Dr. Halliwell has mentioned.
What struck me when we were meeting with the centres -- and you will be hearing from one of them later this afternoon -- is that they are very much local organizations. They are community based. Perhaps, if we are lucky, they might be organized and coordinated at the level of the health region. I cannot speak about what goes on at the provincial level. However, there is clearly no provincial level of data collection in most provinces. That makes it a lot different from most of the data systems we have in Canada, where the collection goes from the province to a national organization, such as Statistics Canada, the Canadian Institute for Health Information or Health Canada.
Because the care crosses from home care to institutional care, those data sets are quite differently organized. There is, perhaps, good information from the institutional care side but not from the home care side. That makes it difficult to get a picture. As we were analyzing our data, one of the major issues was trying to track the patients through various types of institutional care settings and the home care setting, to come up with a complete picture. Even though many patients may want to die at home, some may be in situations where they need to be in a hospital setting.
I would like to address the issue of the administrative databases. I am presently on secondment from Statistics Canada, where I worked extensively with the Canadian cancer registry. We have excellent data on the incidence of cancer and mortality. We are getting data on survival. We have hospitalization data, which are linked within Statistics Canada, that allows us to get care records across patients from about 1992 onward. We have just signed a contract with Statistics Canada so that Health Canada can actually go over to Statistics Canada to conduct further analyses. One of the areas we will be looking at is palliative care.
In terms of statistics, there is a huge gap where home care is concerned. However, the Canadian Institute for Health Information is developing databases that are not yet in place.
Dr. Mills: This brings me back to Senator Beaudoin's question about what kinds of things could be done. A number of years ago, I did a key informant survey in Ottawa-Carleton about the needs for palliative care in the region. One of the key findings that came out of that survey was that there was a need to find some way of ensuring that patients did not fall through the cracks when they went from the home to the hospital, back to the home, to the hospice, or perhaps to an emergency ward for some particular thing. They kept getting lost because there was no single information tracking system. There was no simple way of tracking this information. Some people suggested that a smart card could be used for this purpose. The need for such data is that these people do not stay in one setting all the way through their care. They move across settings. The obstacles to getting coherent data collection, even administratively, are immense. They simply reflect the obstacles to good, continuing, coherent and comprehensive care.
[Translation]
Mr. Halliwell: I agree with Ms Gaudette. Statistics Canada is very much aware of the problem and is working at solving it, so that researchers could have access to the databases. In fact, thanks to the Data Release Project, academics who are working on research projects will have access to the Statistics Canada databases as though they were themselves employees of Statistics Canada.
One of the priorities of the Department of Health, in the field of data processing with the provinces, is to promote the development of a method to identify Canadians when they use the different health services by providing them with an identification card or an identification number. This would lead to much more thorough databases and better links between them. This is more important for the client, but it would also be an important step to providing better access to these big administrative databases for research projects.
Senator Corbin: Can a change in minister affect the nature of your work, in the sense that research or support or service delivery in one field might be favoured over another, and might this be the case more specifically when it comes to palliative care?
If a minister told you that it was important that the department focus quite seriously on one service in particular, on the deficiencies, the opportunities, the regional deployment, and the level of inter-governmental co-operation that would need to be established to ensure a good palliative care system in Canada, I presume that all of the department's bureaucracy would do what it had to do in order to respond to the expectations and the wishes of the Minister.
Is this in fact how it happens? Or is it each branch which decides how important a report such as the Senate report on Palliative Care is? Who is it who makes this type of policy decision?
I do not mean to point the finger today, but I have the feeling that despite all the work you have done and all the progress that you have made, things aren't happening fast enough. Could you please tell me about the political and bureaucratic relations in a field such as this?
[English]
Where do you get your marching orders? Are there marching orders?
The Chairman: That is a difficult question for any of you to answer. Perhaps Ms Ouellet could give it a stab.
Ms Ouellet: As a policy branch, we like to think that we have some sense of that.
Clearly, the department has a large mandate and a huge number of priorities. In part, our structure reflects, through our business lines, the fact that we have tremendous pressures and priorities in the areas of risk management and services to First Nations population health and health care. Within the department, there is no doubt that we do need to manage our efforts and resources in all of these areas and probably could not neglect our statutory mandates in this regard.
Having said that, when ministers set priorities, those priorities are, of course, taken on extremely seriously by the department. In fact, we work to present the minister with options and initiatives that will respond not only to the direction of those priorities but to the urgency and speed with which ministers determine that they want to see actions move forward.
Ultimately, our role is to provide good analysis and good advice, and there are any number of other factors that come into play in terms of how quickly initiatives can be moved forward. These include our own resources, our own capacity, and the extent of agreement with provinces and territories. As I am sure you realize, because health care is a provincial jurisdiction, the federal government's role is one of support, facilitation, and leadership, but in conjunction with and very much in collaboration with provinces and territories.
The Chairman: Considering the delicacy of that question, I appreciate your answer.
[Translation]
Senator Pépin: I hear you all talk about the excellent co-operation between the provinces. However, if we are to believe what the witnesses told us last week and what the newspapers reported on the weekend, there are three problems: physical access to the centres, unavailability of drugs to everyone, and shortage in home care workers.
It has been said that depending on the region or the province where you live, you do not or will not have the same care. One of the things that we are looking at is how to ensure that people living in Halifax, Quebec City, Toronto and Vancouver, will have similar services and similar access.
True, co-operation is lovely. However, on the practical side, if you keep both feet on the ground, how can this be organized and how can you coordinate this care? From the testimony we have heard up until now, the quality and the access to this care, as well as the availability of good drugs, depend on the region in which you live. What can we do in order to help you with this job and, more important, so that everyone can have access to the same level of palliative care?
[English]
Ms Ouellet: In many ways, we have uncovered, as part of our documentation of the existing home and community care programs, much of what you talk about. Different provinces currently offer quite different access, at least in terms of publicly covered services. In some provinces, the access to services will concentrate primarily on professional services, and within that, primarily nursing services. In other provinces, other jurisdictions, they may have a very comprehensive range of services.
In many ways, the state of our current home and community care services has depended upon a number of things. It has depended upon how the provinces themselves have chosen to organize their own health systems, where they have chosen to put the emphasis, and in many ways the resources that they have had available within their health budgets to develop the home and community care sector. In other cases, it has been perhaps a matter of a decision, politically or otherwise, in terms of what should be the role of the public system versus the private system.
Home and community care is also an area where one sees a very high level of privately provided services. Much as my colleagues have been talking about information, while we do not have good information on the publicly provided services, our information on private services is much less -- although perhaps not quite zero. Finding the information would involve interacting with a number of private providers at a community level all across Canada. It is very difficult to have a handle on what those services are.
From the point of view of what we can do to facilitate and promote the availability of these services, the federal role is to work together with the provinces to identify what are the issues and challenges, and which of those issues are more national in their context. Certainly, some of the challenges with respect to health -- human resources, providers, professionals -- are issues that are common across jurisdictions, as are issues with respect to information systems and the quality-of-care standards. We are attempting to work with the provinces to deal with some of those national issues.
In so doing, we find that, at least conceptually, there is quite a degree of consensus about the kinds of home and community care services that we would like to see in the future. At this point, there is a question of resources within the jurisdictions. There is a question of other preoccupations with other pressures faced, particularly on the hospital side. Some jurisdictions, therefore, are prepared to move faster than others in this area.
The minister's impetus to bring his colleagues together to talk about this is one of the ways in which we can help move the discussion along. Federal and provincial ministers already agree -- and this would have been the piece of the discussion that you would have missed -- that this is an area of priority. They realize that this area of the system is under the most pressure and will feel most the implications of an aging population. We need to look at this sector and improve services; but at the end of the day, the decisions on how those services are delivered and organized and how quickly those services can be expanded to meet the needs of Canadians will rest back with the provinces.
[Translation]
Senator Pépin: It is not unusual these days to see members of a family leaving their home province to go and work in other provinces. So it is quite probable that they would suffer from similar health problems and yet not receive the same care because that care varies from one province to the next.
[English]
Ms Ouellet: That is true and it is because of another complication within our system. Many provinces, with the exception of Ontario, have chosen to regionalize the service delivery. In effect, this means that the provinces provide regional health authorities or community health boards with global budgets to provide services to their populations. One can see variability at a regional level within a province, depending upon how that particular region has assessed the needs of its constituents and how it has chosen to emphasize some services and not to provide other services.
Within a general overall accountability framework, there can be some variability even within provinces.
[Translation]
Senator Pépin: Could we find the same thing here with the use of certain drugs? Could one province decide to restrict the use of certain more costly drugs unless the patient has private insurance? Are some provinces more likely than others to use specific drugs?
[English]
Ms Ouellet: Certainly, we will find some variability between provinces in terms of their drug plans for publicly covered drugs. Within a province, however, because that is still managed at a provincial level, eligibility and co-payments or deductibles would be consistent across the province.
Ms Gillis: I had mentioned earlier that the province of residence is not a determinant for whether a First Nations or Inuit person can access any drug. It depends on the prescribing physician. Any drug prescribed by a physician that relates, especially, to pain management and control in the home would be funded under the non-insured health benefits program for First Nations and Inuit.
There is a wide range of drugs on the formulary. If a drug is not on the formulary because it is usually of very limited use, we do have a process whereby the physician can apply and receive a quick turn-around through a drug centre. In speaking to the people within the branch who manage the program, the pharmacists say that, on such issues, the people are not refused or turned away. People do have full access to the drugs.
The Chairman: Dr. Mills, you said that 90 per cent of palliative patients are cancer patients. One of the things we talked about in our original report was the need to broaden palliative care to cover not only cancer patients but also victims of ALS, Alzheimer's and other diseases. I gather from your information that you do not think that that has happened to any great degree over the last five years. Am I correct?
Dr. Mills: It is not so much that there is any preferential delivery of palliative care to cancer patients. Rather, cancer is so much more common than any of those other conditions; it tends to occupy the capacity for care. Canadians have a 1 in 3 chance of developing cancer in their lifetime. That is a lot of people with cancer at any given time. Of those people with cancer, a certain proportion of them will be requiring palliative care compared to any other condition that ends up requiring palliative care. For the foreseeable future, cancer patients will be the dominant clientele of palliative care. Of course, you are right; it is not the only clientele and we must ensure that the services are appropriate for all people who need palliative care.
The Chairman: We actually found anecdotal examples in our previous study where people could not access palliative care, even if they needed it, because they did not have cancer. The criterion at the door was this: If you have cancer, you get palliative care; if you do not have cancer, tough.
Ms Gaudette: Of the six centres that we studied, only one specifically restricted its program to cancer patients. Most of the programs did accept other patients. There were some interesting discussions around the table a few weeks ago regarding the relative need of cancer patients for palliative care.
Metastatic cancer is often associated with severe pain. It is a prolonged process and the curative cancer treatment is normally provided in a central cancer agency for therapy or in treatment centres that may be a long distance from the patient's home. Towards the end of a cancer patient's life, he or she is usually treated nearer their home and so may be moved to a palliative care setting if they are lucky, as you say.
The Chairman: Ms Gillis, with respect to aboriginal care, I was somewhat surprised -- and maybe I did not hear you correctly -- to hear you imply that this program for community-based care will not take effect until 2002-2003. Did I hear you correctly?
Ms Gillis: The program was announced at $152 million over three years. The funding ramps up. The ongoing funding begins in 2002-03. This year, there is funding and they are beginning their planning. Next year, there will be more planning, development and service delivery in areas that are readily available. That includes training of all the health workers, addressing some of the capital needs, and so on.
While services will be delivered as the program is being developed, each community will be developing as needed at their own pace. However, the full funding does not come into place until 2002-03.
The Chairman: I am from Manitoba. All aboriginal children in Manitoba who have a serious illness are brought to the Children's Hospital in Winnipeg. In many situations, an aboriginal child cannot be returned to his community because there are no services in place in that community.
We all know that acute care hospital beds represent the most expensive health care delivery system; we do not have to go through that argument again. That is a given. However, we use the most acute care to look after an aboriginal three-year-old who would be happier and would have more stability in his life if he was home in his aboriginal community. I assume that those are the kinds of things you are attempting to address; correct?
Ms Gillis: You are absolutely right. In Manitoba, in particular, Medical Services Branch, Health Canada, the Department of Indian Affairs and the Province of Manitoba have initiated a special program related to First Nations in Manitoba. The program works with a number of children who have needed high levels of medical care and have been placed in hospitals and in special care for a period of time. The mandate of the program is to move these children back to their home communities and to put in place, in many instances, 24-hour support services. This is a special pilot program outside of this new home care initiative.
In addition, there is a significant amount of pressure in First Nation communities -- they want to get this program off the ground quickly. They also recognize the importance of planning the program well, ensuring that the foundation is well based so that the program can continue into the future successfully. There are great pressures, and communities are feeling those pressures. We are working with them to help move this along as quickly as possible.
The Chairman: Perhaps some of the letters that I wrote will have an effect. One never knows.
[Translation]
Senator Beaudoin: When it comes to health, federal and provincial government relations are very important. Each has a role to play, the federal government, for example, when it comes to the criminal code, spending power, et cetera.
You say that there are monthly meetings between these two levels of government. What are the provincial governments telling you? Are there conflicts? Are they satisfied with what is happening across the country? I presume that provinces do not all have the same system, some of them may have more money and find it easier.
Canada is recognized around the world when it comes to health care, but there is no such thing as a perfect system. What do the provinces criticize, and what do they praise?
[English]
Ms Ouellet: That is a big question.
Senator Beaudoin: You may restrict it, if you wish.
Ms Ouellet: When I said that we meet monthly, this obviously is not the same group that meets that frequently. What I meant to indicate is that there is, within the structure of federal and provincial committees in health, committees of ministers, a committee of deputy ministers, and four advisory committees. Within those structures there are also some subcommittees on specific topics, one of which is the topic that we are discussing today, home and continuing care.
In order to do the business of trying to advance work in health and, more particularly, in the health system across the country, these committees do meet very frequently. The mandates obviously flow from agreements of ministers and, in this particular case, there is no argument that home and community care is a priority and that this is something that we should work on. In fact, that has accelerated in some ways the frequency of our meetings and of our conference calls on this particular subject.
Essentially, provinces want to know what we can help them to determine about what works and what does not work in terms of effective models for delivering care. Provinces are interested in looking at what kinds of cost efficiencies they can build into the system. Therefore, for example, in this area, we have a study that we are funding through the health transition fund, which I have mentioned already, that is looking at the cost effectiveness of home and community care: For what patients and in what situations is this cost effective, and when is it not only not cost effective but not appropriate in terms of the levels of need of the patients?
We assist the provinces with supporting demonstration projects with research. We help to facilitate the exchange of information. We help to develop strategies on moving forward, even when those strategies are really primarily within their own jurisdictions, and it is up to individual provinces to decide when and how quickly to move forward on those initiatives.
By and large, the difficulty is that, while the challenges are quite common, the provinces are at different points in terms of the development of their own systems, and their readiness to move forward is not all at the same level at the same time. However, where we can, we support that. Enough funding for health care is always an issue, but even the provinces would say that more funding to do the wrong thing is not what we want to do.
We need to determine what are the best ways to develop this sector so that we know that we are meeting the needs as best we can within available resources. We know the quality of care is good and we can monitor and assess the quality of care that people are receiving in the community. We know that this part of the system is becoming more and more integrated with other parts of the system so that as you leave one setting you do not fall between a crack until some other setting finds you and begins to offer you care.
On a strategic and practical level, there is work that is underway that will be helpful. At the end of the day, the federal government can certainly play a role in collaboration with the provinces in most instances.
The Chairman: Thank you very much. I thank all of the panellists today. We are hoping that you will be available for us perhaps on another occasion if we have more questions, either by letter or by personal appearance.
Ms Ouellet, you promised us a summary on the interbranch committee with respect to some of the work that we have been doing.
Mr. Halliwell, you indicated that you would be giving us some summaries -- and then full studies, if honourable senators would then like the full studies. I have already seen some of the studies from the NRDP.
If any of the rest of you think that there is material that would be useful for our deliberations, please do not hesitate to send it to us. I will ensure that it is distributed to all members of the committee.
Senator Corbin: Before Ms Gaudette leaves, I wish to raise a grievance. Members of Parliament who wish to obtain analysis from Statistics Canada must pay for it. I have had to pay for information from Statistics Canada. You now tell me that university researchers, under the guise of being associated with Statistics Canada, can access your information banks at no cost.
We heard earlier that a client department like Health Canada has a contract with Statistics Canada. I do not know if there are costs incurred or not. However, Madam Chair, in the pursuance of our duties and our work as responsible members of Parliament, I do raise a grievance that we should not have to pay for information that is crucial to our evaluation and assessment of government programs.
The Chairman: Your grievance is heard and I am sure that, at the appropriate time, the appropriate people will be told. Thank you all very much.
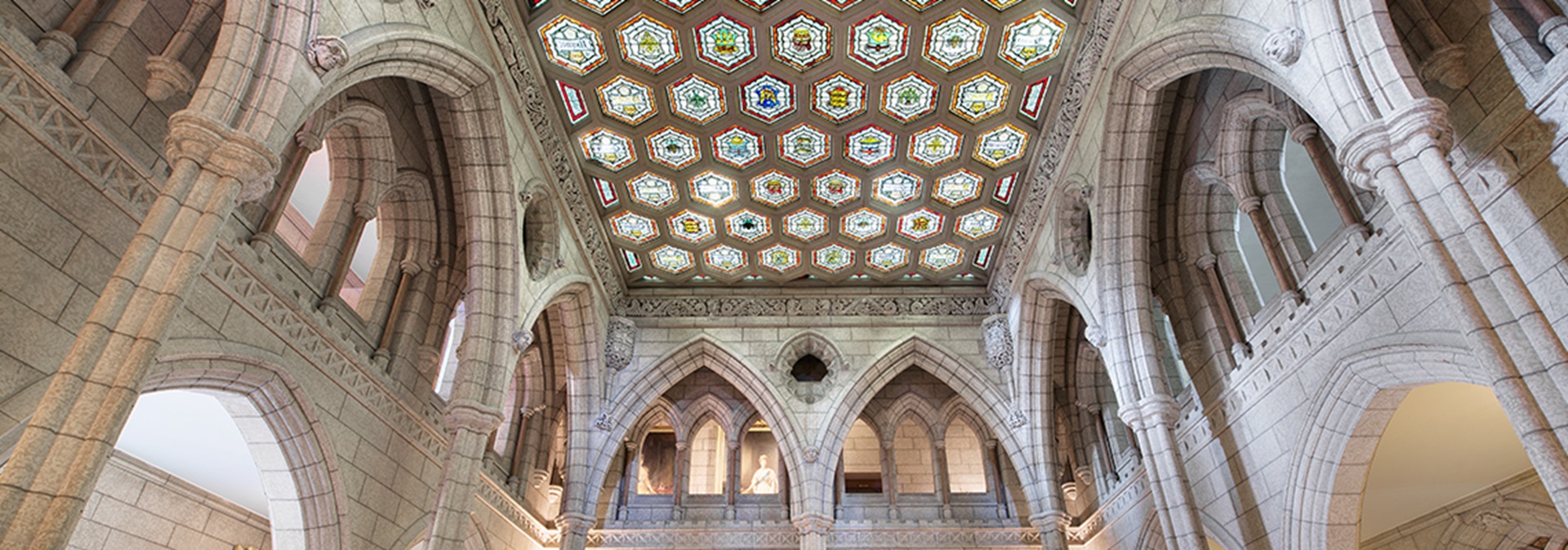
Honourable senators, we are extremely fortunate to have with us some guests from the Elisabeth-Bruyère Health Centre. Any of you who live in the Ottawa area understand the positive work they do there. I have known some people who have been there and who have died there. On behalf of them and their families, I wish to thank these witnesses and the staff of the Elisabeth-Bruyère Health Centre for the wonderful care that is given.
With that personal endorsement, we have at the table today Dr. Ray Viola, Dr. Cori Schroder, Ms Maryse Bouvette, and Ms Diane Hupé, who are all with the Palliative Care Program.
Ms Maryse Bouvette, Nurse, Coordinator, Pain and Symptom Assessment Team, Palliative Care Program, Sisters of Charity of Ottawa Health Service: Honourable Senators, we represent the Regional Palliative Care Centre, which includes 45 palliative care beds located at the Elisabeth-Bruyère Health Centre, which is part of the Sisters of Charity of Ottawa Health Service. This also includes a 24-hour phone consultation service and a home consultation service, as well as the Institute of Palliative Care. All three components are part of the Regional Palliative Care Centre.
One way to share some of our experience and concern with you is to describe a specific case. We hope that taking you through this case will give you an appreciation for the type of concern we feel. This case involves a 45-year-old mechanic named John. He was diagnosed with cancer of the lung. He has two children, two boys aged 12 and 15, and his wife works part time. When he first received his diagnosis, he was treated with surgery and chemotherapy, as well as with radiation treatment. He is now having a recurrence of his disease, and his oncologist offers him a second-line chemotherapy treatment.
The real goal of this chemotherapy treatment is symptom treatment and symptom prevention. There is a potential for the prolonging of life of approximately a month or two, but John decides to decline that second-line chemotherapy because of all the side effects he had from his first experience with chemotherapy. His oncologist refers him to the palliative medicine clinic at the cancer clinic so that he can get advice on symptom management and pain management and also be provided with information around palliative care or related to palliative care issues.
A month later, John is presenting with major shoulder pain. The pain is moderate to severe, it is burning, it is sharp, it is there all the time. The pain prevents him from sleeping because it is bad during repositioning. It is worse during coughing. It is also worse during deep breathing. The family physician recommends a chest x-ray to see what is happening and prescribes some regular morphine and, on an as-needed basis, a dose of morphine to help with his pain. He also seeks help from the palliative medicine clinic where John was seen in the first place. The family physician requests and obtains a consultation with the physician from the palliative medicine clinic.
John is seen by the palliative care physician, and the x-ray shows a large mass involving the ribs, which certainly explains some of the symptoms he has been presenting with. Other symptoms, such as nausea and constipation, are also recognized. The palliative care physician recommends increasing the dose of morphine and adding some co-analgesics, medication that is not really an analgesic but that could help with some pain. John is also to have another assessment with the radio-oncologist for some potential radiotherapy that could help with symptom control.
At the same time, as the picture is worsening the family is having a hard time, and so is John. It is a good time to have the Community Care Access Centre involved. A nurse was not needed previously, but now one is required to check regularly on his symptoms and pain, and a social worker is involved to help with psychosocial and spiritual issues. A physiotherapist is also on-board to help with positioning and to bring a non-pharmacological approach to help with pain management. The family is also offered volunteer services through the hospice involved.
John and his family are willing to accept any kind of help because they really need it. The wife is still working, so it is great help to have all these people come into the home to help and bring a sense of security that John is not alone for a long period of time.
Despite the fact that the symptoms improve, John's situation continues to deteriorate. As John becomes weaker, the family physician agrees to do home visits. Another symptom arises: a bad case of shortness of breath. It causes a lot of anxiety. At this point, the family physician asks for a home consultation to help the situation. The nature of the symptom is causing a lot of anxiety and the family wants it corrected. The palliative consultation team goes into the home and addresses the symptom of shortness of breath by administering morphine via a pump for a continuous delivery of medication and adding medication such as steroids and some oxygen to it. The nurse is there to teach the family about non-pharmacological approaches to control the anxiety, such as relaxation breathing, companionship and relaxation. That certainly helps, as does some medication administered to lessen John's anxiety.
John's wife then decides to quit her job because it is necessary for her to be around John a lot more. This causes some financial issues. However, the social worker is there to try to assist with that, as well as to support the two children. As time goes on, John becomes less and less conscious and John's wife is very worried that he is not eating or drinking that much. The idea of dehydration is then an issue. To address it, we are able to bring about some hypodermoclysis -- that is, hydration under the skin -- in the home setting. That helps the wife to know that at least he is not dehydrated. We also have to look at the benefit versus the burden of this procedure. It is done with the idea that if it does not help, we will discontinue the procedure. The nurse also undertakes a close follow-up on the mouth care -- that is, the good hydration of the mouth -- and teaches the family how to do it as well.
Things settle down until the next symptom arises: agitation and restlessness, which we call delirium. Again, the family physician is able to access palliative care expertise to look at the management of it in the home setting, which works well.
It was decided at the beginning of the disease that John wanted to remain home for as long as possible, but he did not want to die at home. Although his symptoms are under better control, his deterioration is obvious, so there is a planned admission to a specialized palliative care unit. John dies three days after his admission to the palliative care unit. After his death, some work remains to be done with the family. Bereavement support is available not only through the hospice setting but also through the specialized palliative care unit by phone calls, by memorial services, and by bereavement support group.
That is but one story. They are not all that well coordinated, but it would be preferable if it could always happen like that.
I am here to share with you the clinical care and the team work that is required for the care of a person who is diagnosed with a terminal illness. I have some key points with which I should like to begin. First, there are the patient's needs. Patient and family are part of the team, so they need to have access to information and to have a chance to share their concerns so that they can have and make informed decisions.
Second, access to interdisciplinary palliative care expertise is essential. Patient and family represent a unit of care. We need to be there to help them follow their goal. "Quality of life" depends on their own value of that phrase, and it is very individualized. The health care team members are key to recognizing the needs and initiating the services that are available, when they are available. Ongoing collaboration between the oncologist and the family physician is crucial. An interdisciplinary and holistic approach is essential to address their needs. "Holistic" means overall -- not only as a person in a body but also as a psychosocial, emotional and spiritual being.
John's case can be used to bring out some of those points. In this case, John was well informed. He had options. He decided about his treatment, about where he wanted to journey with his family, and about where he wanted to die. Often, dissatisfaction related to patient care is due to the fact that people are not always well informed and they do not have a chance to make that decision.
Family physicians are essential. Individuals cannot dream of dying at home if there is no family physician with them in a home setting to do home visits. However, many physicians neither feel comfortable with that nor want to do home visits. In my experience, I have learned that, sometimes, physicians will change their mind because they realize that they have a service there to help them. It is an attitude, almost, that we must change.
The primary care team must have access to expertise. We cannot expect everyone to be an expert, but we can learn. The number of palliative care patients that a family physician may have in one year may not be enough that he can maintain that expertise. However, knowing that there is a team to back up a physician may help a lot. John was privileged in that he was able to access the service and he was well treated at home.
Pain symptom management must be addressed holistically. You may have heard of the principle of total pain. We have been focussing on physical pain, but physical pain can be worsened by psychosocial and emotional issues. That means that a portion of that physical pain can be alleviated by addressing those issues, and not only by using pharmacological approaches.
Collaboration and communication between the family physician and the oncologist is essential. Often, that is what happens in reality. A patient is followed by his family physician. He is diagnosed with cancer and then he is followed by a specialist for a period of months, maybe years. When he reaches, say, the palliative care phase where there is no more chemotherapy to be offered, then what does he do? He returns to his family physician, where he has lost contact for the last few months or years. This is not a seamless system. We need to have the continuity, collaboration and communication between the family physician and the oncologist or specialist.
The interdisciplinary resources must be made available. We may recommend that you need a social worker and a physiotherapist at home, but is that service available out there in the community? Furthermore, are we suggesting things that are not available? We must ensure that they these services are available.
Optimal communication among the patient, family and all the care system is also important. The case that I related to you is a good example of the fact that when good communication happens you can have a good result. The symptoms were well addressed, the care was increased as the disease progressed, and the communication was well established.
There is no ideal place to die. The ideal place to die is defined by each of us, depending on our experience and values and our actual status.
I cannot say how important bereavement support is. It is not because the life of this person has ended that everything is a fait accompli and great. There are still lives happening and they are bringing with them some heritage. We need to ensure that we are there to help them journey and find some meaning. Sometimes, it takes a lifetime to find meaning in events that are happening to us. Certainly, by sharing and remembering, we can help those family members remaining to live better and perhaps have a better attitude towards life in general.
Dr. Cori D. Schroder, Physician, Palliative Care Program, Sisters of Charity of Ottawa Health Service: I am a palliative care physician. I provide clinical care to patients on the unit and as a consultant within SCO. The other hat I wear is that of an educator. As I have a great deal of interest in providing palliative care education, I should like to look, focusing on the case, at the educational and training perspective.
When I think of an overall goal for palliative care educational programming, especially in regional terms, since as we do it on a regional basis here that is what I am familiar with, it is to raise the general skill level of all health care providers and ensure ongoing competency so as to improve the delivery of palliative care to all dying patients in the region. I think there are difficulties and challenges with respect to palliative care education and training. Some of those relate to an appreciation of the complexity of the care that is encompassed by palliative care. Not only does this care involve the physical domain of pain or symptoms, but also the psychosocial and spiritual domains.
Another aspect that adds to the complexity of palliative care is the changing focus of its requirements. Initially, palliative care had a cancer focus, but we are now expanding and looking at other patient populations who suffer from chronic diseases such as end stage heart disease and lung disease, musculoskeletal disease and neuromuscular disease. Gaining sufficient knowledge in those areas has created difficulties. How do we take what we have learned in cancer care and end-of-life care and apply that knowledge to people who have other chronic disease processes?
I believe another aspect of the complexity of care is the setting in which care is provided. We have heard, too, that palliative care goes across settings. It is not only institutional care, but also care in the community, whether within an urban or rural centre, and that adds to the complexity of what we need to teach.
The process involves the acquisition of the appropriate knowledge and skills to take care of these patients. I think of key importance is attitudinal learning, which is extremely difficult. Looking at the issue of pain management, we have spent years training and teaching people about how to us opioids and analgesics appropriately. Until we start changing attitudes, palliative care levels will not progress. We are seeing studies that show that people are not getting good pain control. We are reminded, however, that changing attitudes does not occur quickly and it also does not occur using the lecture method that is the standard approach to education.
I believe that education training in palliative care needs to teach people how to collaborate and work in a team. You have heard about the virtual team in the community, certainly the teams within palliative care units, but people need to be taught how to work in teams and how to collaborate their efforts. That does not come naturally. We need specialty training. It is great if all our health care providers have some basic training, but you need the experts to provide resources in consultation, in education and in research.
We need to evaluate outcomes. We do not know how effective the existing educational programs are because they are not evaluated. The ultimate outcomes must produce benefits to the person in the community who is dying. Only then, once we have evaluation, can we disseminate effective approaches to education.
Last, in looking at regional programming, we certainly need community participation in the planning, the implementation and the evaluation processes. In this particular case, the medical oncologist and the family physician showed attitudes of care versus cure. They showed the importance of sharing the care, of collaborating and of good communication. They had basic symptom control knowledge and sensivity to the non-physical issues, such as psychosocial and spiritual issues. They were aware of resources and when to use them well, and they were able to function within a team.
Where did they learn how to do that? Unfortunately for undergraduate medical students, there is no consistency as to the presence, format or topics for palliative care education, despite the recommendation in the 1995 document. Training as to how to function as a team member to solve complex problems does not exist either. There are some post-graduate medical training programs that do have mandatory palliative care rotations, but, again, the teaching is not consistent. Many, especially family physicians who are going to do the bulk of the care, are not even guaranteed any mandatory training in palliative care. Again, training to function as a team is non-existent.
In respect of continuing medical education, we have, in Ontario, a few small initiatives, but since each year they are still considered initiatives, we never know whether or not the funding is going to come in. These initiatives are sporadic at best, applied differently in different regions and limited by the lack of funding. They are not specific to settings. For example, someone may develop an initiative that works well in an urban centre, but teaching people in rural centres remains in question because the setting of care and what is available to them is very different. There has not been an evaluation of the existing Ontario initiatives because there is no funding and so no interest in doing that at this time.
The palliative care consultant shows expert symptom control knowledge -- again, holistic care. This consultant is very supportive of the primary care team, acts as a resource and an educator, and is very much able to function within the team. Where is this learned? A few centres have been offering post-graduate training. Recently, the Royal College of Physicians and Surgeons of Canada and the College of Family Physicians of Canada have conjointly accredited a program of post-graduate training in palliative medicine. Seven out of fifteen faculties have applied for the program, but there is no funding attached to it.
Senator Corbin: What do you mean by that?
Dr. Schroder: There are no salaries for the residents and no specific funding to build the infrastructure related to that particular program.
The interdisciplinary team members who care for John and his family are as important as the physicians. They demonstrate attitudes of care versus cure, basic understanding, knowledge of palliative care as related to their scope of practice, and the ability to function as part of a team. We do not know where they received such training. For nurses, social workers, pharmacists and pastoral caregivers, there is no mandatory palliative care component to their training. There is limited continuing education, and interdisciplinarity is not taught. For non-professional caregivers, such training is even more limited. We need basic competency of all health care providers to ensure that all people have the quality of care experienced by John. We need funding for specialty programming, and we need support for initiatives that are going to provide the training opportunities to all health care providers. The training must be setting-specific and must reflect the interdisciplinary nature of palliative care. Above all, we need evaluation of the education training programs currently in place in order to assess their effectiveness.
Dr. Raymond A. Viola, Physician, Palliative Care Program, Sisters of Charity of Ottawa Health Service: I will address the research and evaluation components of palliative care programs in this country.
Health care progresses and improves because of research and evaluation. When those do not occur, health care languishes and becomes irrelevant to the population it serves. Research may be simple, such as clinical observation and documentation, or it may be quite elaborate, such as multi-centre randomized control trials.
Palliative care is a young and still developing area of health care that has made great progress in a relatively short time because of the ability of the clinicians in this field to be innovative in caring for the dying and to observe carefully the apparent effects of the innovations they implement. In this way, for instance, the treatment of advanced cancer pain was revolutionized during the last 30 years. The effectiveness and safety of treating John's pain with morphine and other medications was informed by the vast experience of palliative care clinicians during the past three decades. The use of regular doses of morphine by mouth, the use of rescue doses of opiates, the gradual incrementation of doses, and the use of continuous infusions of medications have all evolved from clinical practice, innovation, dedication, observation, documentation and reporting by clinicians caring for the dying.
A similar elucidation of therapies for assessing and managing other symptoms has occurred. For instance, troublesome and frightening shortness of breath is a common symptom experienced by the dying, as John experienced. As well, delirium is very common as death approaches. Advances have occurred in the assessment, prevention and management of these problems, although not to the same extent as has occurred for pain. Weakness, loss of appetite, and loss of weight are enormously common in the dying, occurring for months before death. We are not yet close to being able adequately to help dying persons who endure those problems, nor to help them live satisfactorily with the severe debility that results.
The question of whether fluids should be provided by needle when a person is close to death and has limited intake by mouth is controversial and was faced by John's family and professional caregivers. Understanding the specific clinical issues is important, but equally important is understanding and supporting the decision making of patients and families facing the end of life. That has only started to be explored in a systematic way by end-of-life researchers, and much more work needs to be done.
The impact of caregiving at home by the family of a dying person is enormous, with some of the effects described in our attempt to tell John's story. However, a detailed understanding of the best ways to help families provide this care, especially in the post-health-care-restructuring era, is urgently needed. What are the effects of caregiving on the bereavement of adults and children? What are the short- and long-term financial implications? Which services are needed and which are redundant? How can the patients' and families' preferred places of care and death, most often the home, be realized? How can we best help survivors before the loved one's death and then during bereavement? All of those questions are faced daily by palliative care teams and researchers.
However, most, although not all, end-of-life research that has been carried out has been at the level of clinical observation and anecdote. That has not changed much in Canada during the past five years. Carefully planned and executed studies providing stronger evidence of therapeutic effectiveness or of the multi-dimensional experiences of the dying have been difficult to carry out. Much of the evidence we rely on to treat physical symptoms is extrapolated from stronger research done with other populations of patients. The applicability to the dying is presumed, but not proven.
For continuing progress to occur in the care of the dying and their families, there is now a need to carry out a much larger volume of research and to plan studies that provide valid, reliable and generalizable evidence pertinent to the care of the dying. There is a need for this research to be done in Canada so that it can be applicable to the Canadian health care system and Canadian society. Along the same lines, programs also need to participate in high-quality evaluation processes for the services they provide.
Obstacles to palliative care research are numerous and include the following: the belief that research with dying persons and their families cannot be done; ethical concerns that such research should not be done; the lack of adequate, specific funding for research in palliative care; the lack of trained researchers in the field; limited access by researchers to enough dying persons to carry out the studies; and the lack of relevant, practical and validated outcome measures.
Research with and for dying persons can and should be done. Otherwise, we will never know how to improve the care of the dying and their families and how best to address the complexities and the interactions between the physical, psychological, social and spiritual aspects of suffering.
Research and evaluation are occurring, although in relatively limited amounts and only in certain settings. Some progress has been made in developing outcome measures relevant to palliative care, but the progress overall has been slow. Research has become much more acceptable in palliative care settings during the past few years, but the palliative care team's ability to do the research and evaluation is limited. For clinical programs to carry out research and evaluation, they require researchers with appropriate training and adequate protected time. Without that, clinical and administrative work dominates the time available so that research is not addressed. Most programs have limited funding that barely allows for the clinical work to be done, let alone the education, research and evaluation. The few existing protected researchers often have to work on their own, with few additional resources and with difficulty accessing consistent research project funding.
For end-of-life research to advance, funding must be available consistently to programs that can lead the research. Currently, most funding is internal and, hence, limited to a few programs and small amounts. The training of researchers who are interested in end-of-life care must be increased so that appropriate expertise is available to lead this work. A network of palliative care programs across the country must be developed and supported so that studies involving enough patients can be successfully completed to provide definitive answers to important clinical and health service questions. Recently, such a national network received $60,000 per year of infrastructure funding from the Canadian Cancer Society and the National Cancer Institute of Canada, part of the Sociobehavioural Cancer Research Network. That is a small start.
Clinicians, researchers, patients, families and the public all need to take part in the research planning so that relevant, valid, efficient studies are undertaken and completed. Existing and new programs also need to evaluate the services they are delivering so that continuing improvements in services can occur.
In conclusion, the future of end-of-life care and palliative care in Canada depends on our ability to continue to seek answers to important questions pertaining to death and dying. A sustainable, made-in-Canada research program is vital to the continuing development and existence of credible palliative care in this country. Without that, the pace of development will be too slow to keep up with the health care needs of Canada's citizens.
Ms Diane Hupé, Nurse, Vice-President, Palliative Care Program, Sisters of Charity of Ottawa Health Service: I should like to address the issues of coordination and integration, which are very hard to separate from care. I shall address them from three main perspectives, the first being the interface of specialized care with primary care.
From the case study that Ms Bouvette mentioned, which showed an optimal level of care, we see that the oncologist refers the patient to palliative care once no other treatment for recurring disease is provided. The patient has the opportunity to discuss oncology treatment options with his family physician, and the family physician and the primary care team are actively involved in providing ongoing symptom management with the help and support of a palliative consultation team.
The reality, unfortunately, is all too frequently much different. Patients are too often referred to palliative care once the proverbial verdict of "nothing more can be done" is given, and palliative care is seen as a last resort. There is generally a lack of communication between cancer care specialists and family physicians. It is not uncommon for a patient who can no longer benefit from oncology treatment to be returned to their family physician who has not been informed or involved and who must suddenly take over the complex care of a terminally ill patient. It is no wonder that family physicians are often hesitant to assume the care of a terminally ill patient at home. A lack of knowledge, the heavy time commitment, poor support networks and limited remuneration all contribute to that situation.
It has already been said that access to palliative care specialized teams, especially for consultation in the community, is very limited and in many areas, especially rural areas, non-existent.
From the perspective of the interface of specialized care and primary care, the following recommendations are made. First, there should be integration and earlier involvement of palliative care as an essential component of ongoing cancer care. The same should be applicable for other life-threatening illnesses. This speaks to a change of philosophy that palliative care is not just for the last weeks of life. Second, we need recognition of the key role of the family physician and the other members of the primary care team within the whole continuum of care delivery. They are there to provide basic end-of-life care. Third, to help them, the family physician and the primary care team should have access to palliative care specialists whether they are in an urban or a rural area.
The second perspective I should like to raise has to do with access to palliative care no matter in what setting, and that within an integrated delivery system, as your report recommended. In the case of John and his family, palliative care consultation and advice was available through a variety of means -- an ambulatory palliative care clinic, telephone advice, a consultation team providing home consultations, and bereavement follow-up for the family. It seems that John received appropriate primary and specialized palliative care in a timely manner in the setting best suited to meet his needs and those of his family. Care delivery seemed to be well integrated to provide a seamless continuum of care.
What is the reality? Palliative care is not available and not accessible in many settings and in many areas of the country. Some examples include the following. Many acute care hospitals, especially since restructuring, lack the basic funding to maintain core palliative care teams of a nurse and a physician, let alone an interdisciplinary team. In many regions, there are few consultation teams available to do consultation in the home or in long-term care facilities. Again, this is especially critical in rural areas. There is a significant need for community hospice services that can provide visiting volunteers, day programs and respite for families. As a result, there are significant unmet needs for simple pain and symptom control in addition to unaddressed psychosocial, emotional and spiritual needs.
The delivery of the limited palliative care currently available is too often fragmented, poorly coordinated and difficult to access for patients and their families. There have been important contributions by some communities across the country in developing integrated delivery systems in Edmonton, Calgary, Winnipeg, Montreal and Ottawa. However, those are more regional projects than the result of provincial long-term planning initiatives.
From that perspective, we recommend that provincial governments and regions learn from the experience of the few existing integrated models and that they evaluate them. We need policy direction and funding to develop and provide essential palliative care services at a regional level. Furthermore, components of palliative care services must be well coordinated and integrated for optimal delivery within the overall health care system. As well, mechanisms must be developed to facilitate this integration. Examples would be common standards, clinical guidelines, information, access to facilitate the movement of patients, optimal use of technology and standardized assessment tools.
The last point that I should like to raise has to do with community care, including support to the caregiver. In the case of John and his family, the patient received home care services, that is, nursing visits, home support, medication and the supplies and equipment that he needed within the service limits of the home care program in his area. Because of a lack of extra health insurance for additional nursing services as John's condition deteriorated, his wife had to quit her job, thus adding to the already high physical, emotional and financial demands of caring for a dying person at home. That says nothing of the care of the children that must continue and help them cope with their father dying.
In this case, their family physician and primary care nurse are caring for the patient, managing the symptoms and supporting and teaching the wife in her caregiver role. They are supported by an interdisciplinary team who can do home visits. As the patient's condition deteriorates, and respecting his wish not to die at home, there is a bed readily available in a specialized palliative care unit.
What is the reality? In the last few years, health care has undergone a shift to the community and the wish of the terminally ill to be and even to die at home is well documented in the literature. The delivery of palliative care in the community is seriously impeded by a number of factors. The overall funding is insufficient in home care. The delivery structure is too rigid for the 24-hours-a-day care requirement of a terminally ill patient at home.
Frankly, health care still largely remains focused on hospital care. The scope and availability of home care services varies largely from region to region and from province to province, as you have already heard. The current delivery system does not support continuity of care. To give you an example, rather than a primary care community nurse caring for a patient, as in the case of John, it is common to see numerous nurses from different agencies providing care to the same patient. That is largely due to a serious nursing shortage that is only getting worse. This shortage is certainly worse in the community. As well, there is a rigid system of service allocation, all of which makes for significant fragmentation, real risk of mismanagement of a case and additional burden to a family who must deal with so many service providers.
With the shift to community care, there is the underlying assumption that family will take an active role in providing the care. That is certainly the case for the family of a terminally ill patient. The physical, emotional and financial burden is tremendous on the caregivers. There is very little respite available to support them. Often, there is no insurance coverage for additional services, such as nursing shifts or additional home support services. Finally, as was said earlier, not every family physician feels able and willing to care for a terminally ill patient at home and to make home visits.
From that perspective, we would like to recommend the following. We need a national home care strategy with specific standards, for example, on access, as was mentioned earlier by the honourable senator. We need adequate provincial funding and policy for comprehensive home care services with the flexibility to promote and facilitate continuity and comprehensiveness of care. We need mechanisms -- namely proper remuneration and support systems for the professionals providing community care, especially nurses and family physicians. We need services to support and provide respite to the family and caregivers, such as hospice day programs, respite services, and adequate psychological, social and spiritual support to family, including bereavement follow-up.
There needs to be access to palliative care consultation teams to support the primary care team. As well, there needs to be regional specialized palliative care units for the patients for whom complex symptom management requires hospitalization. Finally, we need a comprehensive evaluation of the cost and benefit of palliative care at home, including indicators of quality of life and burden of care.
I should now like to sum up and capture in a few statements what our team has tried to highlight through the discussion of the story of John and his family, approaching it from the perspective of clinical care and the team, education, research and system integration. The case of John illustrates what should optimally happen in the provision of end-of-life care. If we were to sum up our recommendations into one recommendation, it would be the following: universal and integrated access to palliative care expertise at the end of life for all patients and their families.
Under that, what is truly important, we need a primary care team, especially the family physician, the nurse in the community, the long-term care facility, and other team members, who obtain as part of their basic training the knowledge, skills and attitude to help them care for terminally ill patients.
We also need to support that team of palliative care experts. We need research and evaluation in order to provide evidence-based and effective quality of life and quality of care. We need those services to be coordinated and integrated, and there is certainly a need for policy direction and appropriate funding, the glue that will bring those services together.
The Chairman: I am not sure I will ask too many questions this afternoon because I agreed with everything you had to say.
[Translation]
Senator Pépin: I agree with everything you said. I have followed everything very well, and I think the fact that you presented a clinical case is very helpful to us.
However, there is one thing that aroused my curiosity: When it comes to clinical research, it was said that there were an insufficient number of people dying to allow for a clinical study. How many patients does it take for a nurse or a physician to conduct valid research?
[English]
Dr. Viola: My reference to that was not in terms of the number of people dying but access to those patients who are dying by researchers who are trained to do the type of research that needs to be done.
Senator Pépin: So it is the lack of training.
Dr. Viola: Yes, but also access to the place where the people who are dying are being cared for. The dying patients who need to be included in these studies are not always accessible to the researchers who want to do the work. In Ottawa, we are in a special situation. We have a large palliative care unit with 45 beds, which hosts a number of patients of a particular type. We have a cancer centre that we are closely aligned with and can access. We have teaching hospitals. However, across the country that is not always the case. Even in Ottawa, it is difficult, when we want to do the research, to access the specific patients who would really need to be involved in this. It is the access, not the total number.
Senator Pépin: Someone said home delivery care is too rigid. Why is that?
[Translation]
Ms Hupé: Take the example of health care in Ontario: We are still following the department's policy which states that there must only be so many hours of nursing care provided, so many hours of visiting homemaker support provided, and this is because the budgets are limited. It is very rigid, and that is where my comment stems from, that there are a lot of conceptual changes to be made when it comes to service delivery, when you are looking at health care in general.
Senator Pépin: Are the hours of care provided to patients being limited in order to ensure eligibility for grants?
Ms Hupé: This is still the case in Ontario, and I think in other provinces as well. If a family has a private insurance plan that is fairly comprehensive, they can use this money to purchase additional services, but it is not every family that has insurance which allows this. Many insurance companies have quite rigid policies and will only provide funds for an authorized nurse, when in fact sometimes all the family or the patient requires is visiting homemaker support.
Senator Pépin: Are the drugs programs just as inflexible?
Ms Hupé: Each province has a drug plan for home care patients. Nonetheless there are still access problems for some drugs, among others some narcotics with specific dosages that are not covered.
Senator Pépin: Apparently some family physicians are having problems because they are unable to deal with the house calls they need to make when a patient is dying. Is this because they have not received the right training, or because they are not from the generation of physicians who made house calls, or is it that it is just a different approach?
[English]
Dr. Schroder: I think it is a combination of things. As a result of the work we have done with our family physicians here in Ottawa, we recognize that some people will never do home visits. It is an attitudinal thing, possibly something that is coming with the new generation of physicians.
Senator Pépin: They want to be paid for that.
Dr. Schroder: Some of it has to do with payment, but it is partly a social thing. Some doctors have decided to have a 9-to-5 practice, which does not include home visits. That is a small portion of the family physicians. Most family physicians genuinely want to do home visits. They have a connection with their patients that is incredible. If they are able to follow a patient at home through the dying process and offer the bereavement help, it is as therapeutic for the physician as it is for the patient and family. However, many of them are frightened because they have not received the training. They get into situations in other settings, do not know what to do, and do not have the support and backup that we can offer here.
Some of it is remuneration. That needs to be examined. This type of care is not just going in and dealing with a physical symptom. It involves a lot of discussion, talking and listening. People have to be remunerated appropriately. There are many issues there.
[Translation]
Senator Beaudoin: I would like to get back to the National Health Care Strategy. How can we make this happen? Could it be done by administrative arrangement between Ottawa and the provinces? Would it be possible through meeting with federal and provincial officials? If we want to have a palliative care strategy in this country, then the health ministers will have to come to some understanding and pass an administrative agreement to set it up. I cannot imagine any other way that would work. Both the provincial and federal governments have a major role to play when it comes to health care.
National standards were mentioned, and this is interesting. There is a federal Health Act, that is also interesting, but how will we come up with a strategy? Would it be an agreement between federal and provincial caregivers? What do you foresee? I do not see anything else other than a federal-provincial agreement.
Ms Hupé: The experts who could have answered your questions preceded us. However, I will try to answer your questions. First of all, many terminal patients are at home. This is their wish and this is certainly the way we should be providing health care to them.
Earlier it was mentioned that there were great discrepancies between home care from one province to another. I think it would be important, at the federal level, to establish and recognize that home care services are essential services, in the same way that we do for hospital services. It would be a starting point. And it would provide for basic standards when it comes to access to home care.
Senator Beaudoin: Are you not concerned that a province such as Quebec would say: since health care and home care come under our jurisdiction, give us the funds and we will manage them. This issue must be resolved.
Ms Hupé: Of course under the guidelines that come with the regulations, funding has to be provided, that goes without saying. We need to consider palliative care as a fundamentally integrated part of health care. To this day, palliative care services are still marginal and are not really integrated in the wide spectrum of health care services. I will give an example of a situation that prevails in our region. For a year and a half now, we have been developing, thanks to community and hospital caregivers, an integrated system called the palliative care consortium. In order to help us, we have based it on a small source of funding available through a palliative care association. Lately, the funds have been in real jeopardy.
In our discussions with officials from the Ministry of Health, we learned that one of their biggest problems is the continuity of the funding. The problem is not the direct funding of the care, but rather funding the few positions that coordinate the care. Where should the money come from, to fund this? It is difficult to say. Palliative care does not fit into any of the existing silos -- if I can use the term -- within the Ministry of Health in Ontario. Palliative care services, to this day, are still not considered an essential service needing to be integrated.
[English]
Senator Corbin: I agree with you, Madam Chair, this is an excellent brief.
Dr. Schroder made a comment about continuing medical education that attracted my attention. Last week we heard from the Royal College of Physicians and Surgeons of Canada. Following their testimony and some questioning, I was under the impression that they were on the right road with respect to specialization in the field of palliative care. However, Dr. Schroder, you seem to throw a stick in the spokes this afternoon. I know you do not want to be critical of your colleagues generally. Perhaps it is a misunderstanding on my part. However, the impression I get is that what they are doing is fine as an objective, but it will take much more time and resources before there is a real impact on that front.
The Chairman: Before you answer that, it is important for senators to understand that the representatives from the college actually made exactly the same point as the witnesses, that while there are 15 medical schools, I think they said only four specialized facilities are expected to be up and going this year, and even those four at this point did not have funding. Their concern was exactly the same as yours.
Senator Corbin: The objective is laudable, but could you elaborate?
Dr. Schroder: That would not be continuing medical education, really. Continuing medical education is for once one has graduated and is out practising. I would classify this more under specialty post-graduate training. Some of the physicians who would come back and take advantage of the programs may be physicians who have been practising for a while, but some of them may be physicians who are just completing their residency in family medicine or internal medicine or whatever.
I believe there are seven faculties that have expressed interest in that field that will be up and running. However, the biggest stumbling block is funding in terms of those residency slots. Who will pay the salaries? Also, if you look at the guidelines of what is to be offered in training, there is still developing the infrastructure to be able to offer that. Further, the difficulty is that even if they are up and going and there is funding and each of the four faculties is producing two specialists a year, it will still be a long time before we have a critical mass of palliative care specialists.
The University of Ottawa, through the Institute of Palliative Care, has been training specialists for 10 years as a fellowship. They graduate between one and three persons a year, but that is a drop in the bucket. What happens too is, as they graduate, most of those people end up going to larger centres. Who will serve the rural areas? How will we address the far North and the aboriginal population? It is incredible when you begin to think about it.
The unfortunate thing is re-reading the 1995 report and being reminded of the commitment to education. There is a lot of rhetoric here, but there is nothing in practice.
Senator Roche: I hope that the line Ms Bouvette used -- that there is no ideal place to die -- will find its way into our report. I thought it was very appropriate and telling. I suppose that is right. I would add a proviso that, if you are to die, the ideal circumstance is to be surrounded with love and comfort. In my experience, I think that one would not want to say that love and comfort can be found only at home. Circumstances might preclude that. Love and comfort might well be found in a palliative care centre. Thus, as is evident from all the testimony we have heard, there ought to be more facilities. Virtually every witness has made that point.
Ms Bouvette, you said that, at home, the contact with the family physician is lost for a while as the specialists perform in their areas of expertise. When a terminal situation becomes clear, the family physician comes back into the picture. I took from what you said and from your experience as a nurse that there are many problems with family physicians doing home visits and that that is an impediment to dying at home, because you cannot get the doctor there.
Is it really necessary at that stage to have the doctor present? If home care programs were advanced in this country that ensured the proper blend of nursing care, case workers and social workers for the administration of medicine, would the physician actually have to be physically present to write the prescription, so to speak? He or she does not have to be there to administer the prescription.
I am trying to determine whether we might, in our report, enhance understanding of the values of dying at home by calling for stronger support systems for the family that do not necessarily include doctors. That is the first question.
Ms Bouvette: I think what you are referring to is the possible role of the clinical nurse specialist, for example. I do believe, though, that there is a minimum of involvement of a physician that is required. That does not mean it must always be the physician doing the home visit. It could be a nurse specialist. When I do home visits I do not always have a physician with me. As a nurse, I am able to assess, speak to the physician on the phone and make my recommendation over the phone.
I believe it would be wrong to have a patient followed at home by a team without having the physician lay eyes on that patient on a regular basis. That does not need to be frequently. We could create other sets of problems by doing that. My colleagues may wish to add to that.
The Chairman: Is that partly because there is still that knowledge relationship with the physician and the patient, and the patient really thinks the doctor knows best?
Ms Bouvette: That could be. However, we can build trust, and when we show that we know what we are talking about, certainly that trust can be built. There is no problem.
There is also the fact that, bottom line, a nurse is a nurse and a physician is a physician, even if nurse practitioners are trained to assess well. I hear you loud and clear, and I certainly think there could be a greater role for a nurse specialist to minimize the visits of the physician, be the eyes of the family physician, and assess the patient.
Senator Roche: What I was trying to get at is that I do not believe that the absence of a physician in the home care of terminal cases needs to be an impediment to the person staying at home if the other circumstances are right, if there is enough support care. That is the point I wanted to make.
I want to come back to the question of the relationship of money and education. We are told that the medical schools are only just getting into the training of palliative care specialists, and one of the problems is funding. I think we can perhaps assess the situation by recognizing that society generally has not yet fully understood the value of palliative care. I wonder, though, if the medical profession needs a bit of a boost to push palliative care onto the political process.
I hear the witnesses saying to us, by implication, that our report should be strong in the political process to make the acquisition of funds for this training in palliative care and provision of palliative care a priority. Is it possible that the health care providers themselves have traditionally shied away from this because they go into the training to get themselves ready to be health providers? They want to save lives and see progress. Generally speaking, people do not get involved in palliative care to deal with the dying, they do so in order to promote the living.
I have had a fair amount of non-medical experience with people close to me dying. I sense that the medical profession is uncomfortable with dying, as if it is a failure to cure the person, to make the person well, which is what they really want to accomplish. I think you see my point, that it will not be good enough just for the political processes here to push into the system, although that should be done. The medical profession will need to push much harder -- the medical profession defined as health care providers, physicians, nurses and everyone else -- in order that society get a better understanding of the values of a dying person being protected through love and comfort.
Dr. Schroder: Actually, I can back up a bit and include some of your last question with respect to whether you need a physician if the patient is dying at home. The physician is seen as the person who writes the prescriptions. In fact, that is not the role of physicians. They work as an integral part of a team, and they not only look at the physical issues but they also may be the ones that connect on the psychosocial and spiritual issues. That is why, as a team, it is very important to have all the components. Within the team, then you can decide who does what, and that may be someplace where one can look.
It is true that for physicians the socialization is this cure mentality as we go into training at an undergraduate or post-graduate level. If we cannot cure, then we are failures. As I said earlier, that is part of what we need to be doing in terms of education. We need to start very early on, at the undergraduate stage, and change that to a "care" mentality.
You are right, we could get all kinds of funding for palliative care, but within the faculties of medicine there must be the sense that this is an important part of training. If many of the people who are in the hierarchy themselves are not in that care mentality, then it takes longer. They see this as a question of how to add it into our current curriculum. We have so much in the undergraduate curriculum and post-graduate curriculum, how do we add palliative care?
That feeds into what Ms Hupé said about the need to be integrated and the need to change attitudes. We need to change that socialization of physicians to understand that it is not a failure if you cannot cure your patient. A failure is to abandon that patient. We can start making inroads there. Attitudinal changes take a great amount of work and effort, and you need to start early on.
However, there is hope. In dealing with the family physicians and some of the specialists here, I see that there is a gradual change. There is the realization that we can always do something more for that patient, even if it is only to sit and listen. As a physician, I might not be able to write more prescriptions, but I can sit and listen in order to validate that person, to journey with that person, whether I am a physician or any other member of the team. That is important to understand and get across to the medical students, to the family practice residents, to the internal medicine residents. We need to start and we need to start now.
Senator Roche: I suppose that is right. Pardon my saying, in a friendly spirit, that I have not met many physicians who will sit down and talk. When I am with them I am so nervous about using up their time when someone else may need it more.
It was said here that palliative care has been treated marginally. We are trying to emphasize the priority for it. I am sure the committee will move in that direction. When the cuts in health budgets that were a famous part of the early and mid-1990s took place, did you find that those government cuts in health care had an adverse impact on palliative care? That is to say, did palliative care take a harder hit in the development of all those services precisely because it was seen as being marginal and not central or taking the operation to a high level?
Ms Hupé: You are right. In many settings, palliative care took quite a hit. Because there was no designated funding for palliative care, much of the time it was up to the goodwill of institutions or other organizations to provide some funding for palliative care. When the cuts came about -- that is, the soft funding -- choices had to be made. Oftentimes, that kind of service was removed because it was something that was not funded globally initially.
Senator Roche: Would you say, Ms Hupé, that palliative care suffered, financially speaking, disproportionately to other aspects of health care as a result of the cuts?
Ms Hupé: What is disproportionate is that there was so little funding. Furthermore, it was so vulnerable to start with that any cuts ended up having a major impact.
The Chairman: While you were giving your testimony today, you reminded me a great deal of my parents. They died seven months apart, from very different things. My father had been a minister of health in a province and doctors were part of his group, if you will. Consequently, he wanted doctors around him. On the other hand, my mother was a nurse, and she did not want anyone but nurses around her. You reminded me of that when you were telling your stories.
Your testimony has been thoughtful and concerned. I think it reflects the concerns that most of us have.
Ms Hupé: We have been very honoured to be part of your discussion.
The Chairman: We have two researchers who will address us now. Both of them deal with end-of-life research. I want to make that perfectly clear. Neither of them researches euthanasia and assisted suicide, but some of the research they do asks questions involving those areas. However, that is not their focus. Their focus is on the end of life. I wanted to preface my remarks so that if they get into these murky areas, you will understand that that is not where they are coming from but that, yes, some of those questions do have to be asked in order to get the kinds of answers they require to their other research questions.
We will begin with Dr. Harvey Chochinov, from the University of Manitoba.
Dr. Harvey Max Chochinov, Department of Psychiatry, University of Manitoba: Honourable senators, let me begin by expressing my sincere appreciation for the opportunity to speak to you today. It is hard to believe that so much time has passed since I last stood before the Special Senate Committee on Euthanasia and Assisted Suicide. I hope the intervening years have been good ones for each of you. For those of us working in end-of-life care, these years have been marked by significant activity, some frustrations and disappointments, and ongoing challenges.
As you may recall, my testimony in September of 1994 consisted of telling you about a body of research I have been conducting addressing psychiatric issues in the terminally ill. The contents of those studies are salient to the current proceedings, given that many of them have attempted to understand why some dying patients may covet a hastened death. This research update addresses the Senate's prior unanimous recommendation that research into palliative care -- especially pain, symptom relief, and knowing more about patients who might request euthanasia or assisted suicide -- be expanded and improved. I also thought it important for this committee to see an example of how palliative care research actually looks, so that they can see firsthand how work of this kind can increase our understanding and provide better care for the dying.
By way of a brief review, in September of 1994, I told this committee about a study our group at the University of Manitoba had conducted involving 130 terminally ill cancer patients all receiving in-patient palliative care. That was one of the first and certainly largest studies to look at the epidemiology of depressive illness in the terminally ill. We reported in the American Journal of Psychiatry that, depending on the way the psychiatric diagnosis system was applied, anywhere between 13 per cent to 26 per cent of patients nearing death had a major depression or depressive syndrome. The committee may also recall that I spoke about a study involving 200 dying patients, all of whom were asked if they ever wished that their illness would progress more rapidly so that their suffering might be over sooner. From that study we learned that 55 per cent of patients nearing death endorsed no desire for early death. However, nearly 10 per cent endorsed a moderate or genuine desire for death to come early.
We went on to compare patients with and without a desire for death and we found that the prevalence of clinical depression in those who desired death was over 60 per cent, compared to about 7 per cent in those who did not covet a hastened death. We also found that the prevalence of pain that was of moderate severity or greater was nearly 80 per cent. We reported that patients with a desire for death experienced their families as less supportive compared to patients not reporting a genuine desire for death.
In 1995, Dr. Keith Wilson and I published a model in the Canadian Journal of Psychiatry that looked at the connections between pain, family support, depression, and a desire for death. This model indicates that while pain and family support are important variables, depression is the most important predictor of patients who may covet a hastened death. Thus, while physical symptom distress and social considerations are critical, understanding the psychology underpinning a patient's desire for death appears to be particularly significant.
If clinical depression is present in one to two of every 10 dying patients, it is important to note that fewer than 5 per cent of patients appear to receive any treatment for depression. As such, we published a study that examined several brief screening approaches to help clinicians identify depression among patients nearing death. This slide demonstrates the different screen approaches we utilized in this protocol. It is most interesting that with a single-item screen that essentially consisted of asking patients if they were depressed most of the time, we were able to identify every patient in a cohort of 200 dying patients who was suffering from depression without misidentifying any patient. Thus, we indicate on this slide that the sensitivity and specificity of that screening approach is 100 per cent.
That screening approach was recently cited in a paper published in the February 1 issue of the Annals of Internal Medicine that summarized a consensus panel of the American College of Physicians/American Society of Internal Medicine on end-of-life care. It is our hope that endorsements of that kind will see clinicians more readily identify patients whose suffering, at least in part, may be explainable on the basis of an underlying depressive illness.
Our group is also trying to examine the extent to which dying patients are aware of or able to acknowledge their terminal prognosis. Insight into illness was measured on a three-point scale: those who had no insight, those who believed that their illness was curable, and those who had good insight or full understanding of the gravity of their illness and the imminence of death. As you might expect, we found that most patients were able to acknowledge complete insight, although about 10 per cent denied their terminal prognosis and foreshortened life expectancy. Perhaps most significant, however, is the fact that those who were unable to acknowledge their terminal prognosis and imminent death were also three times more likely to be suffering from depressive illness.
Over the last five years, my colleagues and I have also been trying to study and follow closely the fluctuations that can take place in the will to live among dying patients. Twice daily, patients were asked to indicate on a scale of zero to 100 their intensity of endorsement for various different symptoms, including their current will-to-live intensity.
Here are the will-to-live fluctuations in an 80-year-old woman with colorectal cancer. Notice that when she first entered the hospital her scores were quite high, indicating the paucity of will to live. That is the data indicated on the left of the slide. After several days of being in hospital, her will to live scores improved until she was very near death, at which time her will to live became very highly fluctuant or unstable.
I have shown the will to live pattern of the same patient along with the temporal changes in her reported pain intensity ratings. The story that slide tells is quite profound. It demonstrates a marked relationship between pain and will to live. This particular example is reported as part of a paper we recently published on will to live in the terminally ill in the September issue of the British journal The Lancet. Nearly 170 patients participated in that study.
This slide indicates that within a 12-hour time frame, the average maximum changes in will to live varied by as much as 30 per cent to 40 per cent. By the time we looked at maximum average changes occurring in a 30-day time interval, fluctuations ranged from 50 per cent to 80 per cent.
If, as it appears, will to live is something that can change quickly over the course of one's dying, why might that occur? We found that within the first 12 hours to 24 hours of coming into a palliative care ward, a time of transition for most patients, the anxiety rating seemed to predict the largest changes taking place in patients' ratings of will to live. By the time we had followed patients for one to two weeks, depression seemed to be the most significant factor in predicting fluctuation in patient ratings of will to live. Finally, as death was drawing nearer as we followed patients into the third and fourth week of the study, physical symptoms of distress, especially shortness of breath, seemed to account for most of the fluctuations in will-to-live ratings. This provides an empirically based model to help clinicians understand the changing landscape of will to live among patients nearing death.
Recently, my colleague Dr. Douglas Tataryn has been taking the lead on a series of further analyses on a will-to-live data set. As you can see, we have found that some patients are able to maintain a relatively consistent high endorsement of their wish to go on living. Conversely, there are others who maintain a significantly poor or low endorsement of their wish to go on living, thus the high scores on that will-to-live visual analog scale. Three other discernible groups were also noted, including those who sustain a moderate wish to go on living, those who appeared to increase their endorsement of will to live as death approaches, and those who seem to relinquish the will to live as death draws nearer.
The will-to-live maintainers accounted for about 57 per cent and thus represent by far the largest majority of patients in our study. It would thus appear that most people we studied came into hospital with and in fact maintained a high endorsement of the wish to go on living in spite of their terminal circumstances. Eighteen per cent seemed to lose the wish to go on living as death drew nearer. Twelve per cent of patients seemed to sustain a moderate wish to go on living throughout their course, while a small group seemed to actually acquire the will to live toward the end. Finally, the smallest group, but certainly among the most interesting, consisted of those patients who established a lack of will to live.
It appears that there was a disproportionately high prevalence of colon cancer in patients who gained or acquired the will to live and, as you might have predicted, nausea was also highest in this group. Nausea is a particularly treatable symptom in a setting of palliative care, and this may be indirect evidence that treating distressing symptoms, such as, in this instance, nausea, may help dying patients reacquire their waning will to live.
We also found that the group of patients with a sustained lack of will to live was the least likely to be married. In fact, none of those patients with a sustained lack of will to live was married, compared to at least 50 per cent in all other categories. It is also notable that patients with a sustained lack of will to live reported the highest levels of anxiety and the highest levels of shortness of breath. Thus, the evidence would appear to suggest that patients with a sustained lack of will to live may be more isolated and particularly symptomatic. It is also interesting that those with a sustained lack of will to live died soonest.
With funding from the National Cancer Institute of Canada, our group has also been studying the issue of dignity among the dying. Loss of dignity has been cited in several studies as the most likely reason physicians ceded to a patient request for physician-assisted suicide or euthanasia. In fact, it is not uncommon for people on either side of the euthanasia debate to invoke considerations of dignity as lying at the heart of their respective positions. In a study that has thus far evaluated over 170 patients in several palliative care settings, we are attempting to find out how patients define death with dignity and what factors support or undermine their personal sense of dignity. This study should be completed over the course of the next year and will hopefully provide guidance on how to provide better palliation that is sensitive to the dignity of dying patients and their families.
Finally, I will tell you about an exciting study conducted by my friend and colleague Dr. Keith Wilson here in Ottawa at the Institute of Rehabilitation and Development. This study examined 70 patients receiving palliative care whose mean survival was 44 days from the time of study entry to the time of death. Patients were asked about their attitudes toward euthanasia and physician-assisted suicide. Sixty-four per cent of the sample endorsed legalization of euthanasia and physician-assisted suicide while 58 per cent could imagine it for themselves under particular circumstances at some future point in time should they suffer from uncontrolled pain, severe physical symptoms, a diminished quality of life, or find themselves a burden to others.
Of the 70 patients studied, 12 per cent would have requested a hastened death at the time of the interview if it were in fact legally available. Their reasons for coming to this decision included complaints of drowsiness, weakness, a sense of loss of control and loss of interest, hopelessness, and a desire to die. Of interest, nearly 63 per cent of patients with an interest in hastened death had a major depressive disorder compared to only 16 per cent of patients who did not express an interest in physician-assisted suicide and 21.9 per cent of patients who expressed only a possible future interest.
Let me go back to the question of what progress has been made in palliative care research from a national perspective in the last five years. While there have been some pockets of success by way of individual operating grants and a few critical publications, palliative care research on a national basis has made little headway. We have lost some of our most distinguished palliative care researchers and still have not managed to launch a national palliative care research strategy. A Canadian palliative care research initiative, which had generated significant private-sector interest, failed to attain federal funding.
A Health Canada project to develop a Canadian agenda for research in palliative care employed a three-part national consultation service. Amongst their findings were the following: The existing Canadian research infrastructure is currently inadequate to insure the timely production of useful knowledge related to end-of-life care. New research needs to be developed and supported so that they can take their ideas and research activities into the future, enabling advances that will improve the experience of dying Canadians. Failure to move forward on a national palliative care agenda will result in needless suffering well into the next millennium for dying patients and their families.
I have tried to demonstrate that end-of-life care issues, even the most seemingly difficult of issues, can be studied and addressed in an objective fashion. Palliative care research on a broad range of issues is desperately needed if we are to avoid care that is guided either by ignorance or desperation. Quality end-of-life care research provides the knowledge upon which clinicians can base their decision making, enabling palliative interventions that are sensitive to the needs of dying patients and their families.
Let me offer five specific recommendations for your consideration.
First, the Senate committee's frame of reference is essentially end-of-life care. The title of its final report ought to be "The Senate Report on End-of-Life Care in Canada." A slightly more provocative title to consider would be "End-of-Life Care: A Crisis in Canadian Health Care." Either title will avoid the possibility that the thrust of this report be misconstrued to have a euthanasia or assisted-suicide focus.
Second, that this committee advocate for designated funding, perhaps within the CIHR, to serve as an incentive for training and palliative care service delivery and especially to support end-of-life care research.
Third, that all medical training facilities and licensing agencies be required to include the demonstration of competence in end-of-life care as a condition of their awarding certification or licensure.
Fourth, that all health care facilities, including hospitals and long-term care facilities, be required to demonstrate appropriate standards and competence in end-of-life care including regular monitoring, with appropriate outcome measures to assure quality assurance, as a condition of accreditation or the maintenance of their operating licence.
Fifth, that the federal government and Health Canada be held accountable to the Senate recommendations by way of having to produce an annual report on the status of and progress made in end-of-life care nationally.
I believe that these recommendations would go a long way towards achieving the ultimate goal -- that is, seeing all Canadians having access to excellent, comprehensive end-of-life care in their time of need.
Senator Corbin: On a point of order, we did not get the text of the recommendations that the witness just read. I wonder if copies could be made now for distribution.
Senator Beaudoin: Do you want the report to be labelled?
The Chairman: We will get all of those recommendations and then we will put questions to Dr. Chochinov.
However, we will hear from Dr. Singer first.
Dr. Peter Singer, University of Toronto: Honourable senators, each year approximately 222,000 Canadians die. What is the quality of end-of-life care received by these fellow citizens? We simply do not know.
I regret to report that when I speak to groups of health care providers or the public they usually rate their perception of the quality of end-of-life care in Canada as a "C" on a school report card of "A", "B", "C", "D", "E" and "F". This is not an acceptable grade for cardiac surgery, and it should not be acceptable for quality end-of-life care. We need to take a fresh look in this country at how we care for dying Canadians, and we need to take active steps on how to improve on this care.
Your report "Of Life and Death" made a significant contribution. It clarified the distinction between euthanasia and assisted suicide on the one hand and a spectrum of practices, including palliative care, pain control and sedation, withholding and withdrawal of life-sustaining treatment, and advance directives on the other hand. This is a critical distinction, which needs even more reinforcement and public discussions about dying. When you pick up a newspaper, listen to the radio, or watch a television show, if the topic is about end of life, nine times out of ten the specific issue or the case will involve euthanasia and assisted suicide. However, at the bedside of these 222,000 Canadians who die, 99 times out of 100 the issue is not euthanasia or assisted suicide but rather those other practices that you talked about in your report -- palliative care, pain control and sedation, withholding and withdrawal of life-sustaining treatment, advance directives, and so on.
I take no position on whether or not we should legalize euthanasia or assisted suicide. I am quite sure, however, that if we legalized it tomorrow, it would have a negligible effect on improving the quality end-of-life care of those 222,000 Canadians who die each year.
Let me now focus on the recommendations in your 1995 report, "Of Life and Death," dealing with palliative care, pain control and sedation, withholding and withdrawing, and advance directives. In your report, you addressed these issues thoroughly and effectively, but separately. I think the main step you should now take in updating your report is to bring these issues together into a single integrated concept -- quality end-of-life care -- and focus on how quality end-of-life care received by the 222,000 Canadians who die each year can be improved.
What is quality end-of-life care? Several expert groups, including the U.S. Institute of Medicine, have tried to answer that question. My colleagues and I, including Douglas Martin, from whom you will hear tomorrow on the topic of advance directives, decided that the limitation of these approaches was that they all came from the expert perspective. We conducted a research study to ask patients themselves what quality end-of-life meant to them, and they told us that it included three domains: Adequate pain and symptom control, appropriate use of life-sustaining treatments, and support of patients and families. These domains incorporate the varied issues you addressed in your 1995 report, and now there is a research basis for pulling them together into an overarching concept of quality end-of-life care.
We are now at the point where we recognize that 222,000 Canadians die each year, that most people think that the quality end-of-life care they get gets about a "C" on average -- there are pockets of excellence, to be sure, but, on average, a "C" -- and where we have a unified focus defined by patients themselves that can serve as a target for quality improvement. The question now is how to improve the quality of end-of-life care that those 222,000 patients receive. Let us think about that at three levels: clinical, organizational, and health system.
At the clinical level first, this has been the major but by no means the exclusive contribution of the palliative care movement over the last 10 to 20 years. In addition to the specialized expertise of palliative care providers, we need all front-line health workers who care for dying patients to have skills in providing quality end-of-life care.
I am an example. I am a practising general internist in a hospital. Approximately 10 per cent of the patients admitted to a ward like mine die. I am not a palliative care specialist. It is front-line health care workers like me that we need to target in our health care initiatives.
The University of Toronto has recently launched the Ian Anderson program on end-of-life care based on a $1 million donation from Mrs. Margaret Anderson that aims to train 10,000 physicians in Canada in end-of-life care over the next five years. The press release for this is at the back of your package, and I will come back to this in my recommendations. Here is a situation not where I am suggesting that we need more funding; we have the funding. It addresses many of the issues you have been talking about in the last several hours. The question becomes: How can we work together to put it to the most effective use?
Second, let us focus for a moment at the organizational level. During the past five years, quality end-of-life care has become an issue in institutional accountability. Quality improvement methods have been used to improve end-of-life care, and there are very exciting possibilities here, including report cards for hospitals on quality end-of-life care, viewed as an issue in institutional accountability.
I explore many of these strategies and ideas in a paper that I have deposited with the committee clerk. We can return to those during the question period if you like. The general concept is that a quality assurance mechanism exists in health care. It is not often applied to the area of end-of-life care, but it can be, with some innovation. That can lead to wonderful improvements in organizational accountability.
The third level I want to address is the health system. The first level is not an innovation, it has been there for 20 years. How can we improve education and improve our efforts at the clinical level? The second level has been there for about five years. Organizations realize that this is an issue of accountability. I believe the health system level, linked to the idea of quality end-of-life care, is an innovation. I shall present a vision for the future quality end-of-life care, as a population health systems issue.
If you assume that each death and the quality of end-of-life care received profoundly affect the well-being of, on average, five other people, members of the dying person's family, then about 5 per cent of the Canadian population is affected by this issue each year. That is a huge number, much larger than many of the diseases that we think about. We do not think about it in this way for reasons you were discussing earlier; however, it is an important population health issue. Quality end-of-life care should be a measure of health system performance, given its importance.
There should be indicators in reports from the Canadian Institute for Health Information, as well as Maclean's reports based on them, about the health system performance in the domain of quality end-of-life care.
In a conversation with the chief executive officer of CIHI, I asked: "What would you say if I told you there was a quality issue that affects 5 per cent of the population every year and that that issue is not addressed in any of your quality indicators?" He replied that he would be interested. It is this kind of innovative work that needs to be done at that level.
In addition, there should be cross-national comparisons in the World Health Organization's world health report in consideration of the 54 million deaths annually, 46 million of which occur in low- and middle-income countries.
Let me now turn to what the Senate of Canada could do to improve the quality end-of-life care received by 222,000 fellow citizens who die each year.
First, when you update your report, include a chapter entry on quality end-of-life care, drawing together the previous chapters and focusing on how quality end-of-life care can be improved at the clinical, organizational, and health systems level. Second, at the clinical level, partner with us in the national University of Toronto Anderson program, aimed at educating 10,000 physicians across the country. As part of this program, we hope to hold five transformative conferences targeted at specific sectors. One of the sectors we would like to target is the government. We should do that in partnership.
Third, at the organizational level, we should encourage the Canadian Health Care Association or the Canadian Long Term Care Association, or the organizations that set standards for health facilities, to develop programs for organizational quality improvement initiatives for end-of-life care.
Fourth, at the health systems level, we should encourage the Canadian Institute for Health Information to develop population-based indicators of quality end-of-life care and through Health Canada encourage the WHO to incorporate these indicators in the cross-national comparisons of its world health report.
Since the foregoing recommendations require development of indicators of quality end-of-life care and strategies to use the information to improve end-of-life care, we should support the establishment of Canadian institutes for health research, CIHR, and encourage CIHR to fund the necessary research to accomplish this vision.
Honourable senators, I have presented you today with a fresh and innovative vision on how we can improve Canada's clinical, organizational, and health systems performance in quality end-of-life care. The ideas I have presented build on the fine work you have done in your 1995 report "Of Life and Death." Both in the context of your work in this subcommittee and in your future work in the Social Affairs Committee studying the Canadian health care system, you can have an important effect on improving how 222,000 Canadians die each year. Our collective vision ought to be the provision of A-grade quality end-of-life care to these 222,000 fellow citizens and their families.
Madam Chairman, thank you very much. I look forward to your questions.
Senator Beaudoin: Dr. Chochinov, you have suggested the title, "The End-of-Life Care in Canada," and, more provocatively, "The End-of-Life Care: A Crisis in Canadian Health Care."
In my opinion, the word "crisis" is a bit strong. I say that because it is a controversy but not a crisis, and because, unfortunately, we will all die. What would be the perfect French translation of that? I am not too sure. It is very vague, in my opinion. How would it be translated in French?
Dr. Chochinov: I do not know. When I was thinking of the alternative title, I was torn between having the subtitle be "A Crisis in Canadian Health Care" versus "A Tragedy in Canadian Health Care." You point out that, perhaps, it is neither a crisis nor a tragedy because we will all die. It is for that very reason that it is a crisis or a tragedy.
The fact is that all of us will die, yet we know that only a minority of us will have access to comprehensive and excellent end-of-life care. We also know that the quality of that care can only be as good as the knowledge base that underpins it. For those reasons, if access, education, and research is inadequate, it is indeed a crisis and/or a tragedy.
Senator Beaudoin: We are updating a report in the areas in which we were unanimous. How can we object to that? Of course, it is the thing to be done. We should have done it before, and I agree with that. Why change the title?
Dr. Chochinov: There is a good and specific reason for changing the title. I have been reading much of the testimony. I know that there is some anxiety both among some of the senators and the people who have been giving testimony that the thrust of this committee may be misinterpreted or misconstrued as being yet again about the contentious issue of euthanasia and assisted suicide. One of the senators commented previously that, perhaps, the reason that this report did not receive the attention it deserved is that euthanasia and assisted suicide is too hot a political issue and the committee itself was divided. That gave the government as good an excuse as any not to take action.
If we are talking about the unanimous recommendations, we are really talking end-of-life care. Why not call it what it is? Rather than calling it by the previous title, which did address euthanasia and assisted suicide, retitle it so that we know clearly that this is about end-of-life care. Perhaps that will create more of an impetus for the government to take action.
Senator Beaudoin: It is so general that it seems to include everything.
Senator Carstairs: I do not think we should get hung up by this suggestion concerning the title. I suspect it may not translate well into French, at any rate; therefore, we may have to do something entirely different with it. The focus of what Dr. Chochinov is saying -- it is clear and it has come from all of us -- is that we really want to focus on the issues of how Canadians are dying, however we want to title that some time in the future.
Just to refresh the memories of our witnesses and senators, it was never the intention of the committee to study anything other than euthanasia and assisted suicide. It was only when all these other issues came forward in our debate on euthanasia and assisted suicide that we found ourselves in a real dilemma. We felt it was only fair to report all those things because that is what Canadians seemed to be far more concerned about, quite frankly, than the issue of euthanasia and assisted suicide. They were concerned about palliative care, advanced directives, the withholding and withdrawing of life-support treatment, and adequate pain medication. That is how the report came out.
I agree that we may have to re-jig this whole thrust so that people understand what it is we have truly studied in this update of the report.
Senator Beaudoin: The title of a book or a report is very important.
Dr. Chochinov: Because the initial mandate of this committee was to look at euthanasia and assisted suicide, it behooves the committee to come up with a different title, if the thrust of what we are trying to do is, indeed, different.
Senator Beaudoin: As I have said on a number of occasions, I have no problem with anything on which we were unanimous. As to the rest of it, I am ready to discuss that one day, but not today.
Senator Corbin: In his third recommendation, Dr. Singer speaks of transformative conferences. Pardon me, but my culture does not understand what that means. I have not been involved in any such exercise. I think I understand how it would function, but I should like to add also that one of these should be aimed at government. We here are not government. We are parliamentarians. We may be looked at as critics or advisers to the government, but we are not the government. Perhaps you may want to have a transformative conference with parliamentarians generally, and then another one with governments, which might bring them head on into a clash because things are not working right now. Please tell me all about transformative conferences.
Dr. Singer: It is simply the issue that was being spoken about before in the earlier testimony. There are a number of skills that you want to build. However, fundamentally, part of the issue here is people's attitudes toward death. That is a very, very deep cultural phenomenon, which leads in very interesting ways.
Let us return to the discussion we just had, in order to get parliamentarians on the track that you are on, senator. Let us put aside the issue of euthanasia and assisted suicide for a moment, not on any other grounds other than, perhaps, effectiveness, and let us step back and think about our goal as being those 220,000 people. That is an example of a different way of thinking about things in the parliamentarian sector.
I alluded to what the media is doing. The media is another sector that we want to target. As long as 9 out of 10 stories on end-of-life care on television, radio and in the newspapers have to do with euthanasia and assisted suicide, it will be hard to support and sustain an agenda that will really improve the care on the bread and butter issues that affect dying people. Another sector is physicians. Another is the organizations that can promote the ideas that we are talking about at that level.
In summary, what we have in mind in response to your question, senator, is that rather than large continuing-education conferences, where the emphasis is on getting 500 people and teaching them something, we want to target, in each of these conferences, key decision-makers and take them out of the box. We want to introduce different ways of thinking about these things. Frankly, it is to break the deadlock that has stifled innovation and improvement in end-of-life care, some of the issues that we were talking about. By transformative conferences, we are trying to strike the issue of attitude and conceptualization of the problem. I have presented a very different conceptualization of the problem from other versions that you may have heard.
Let us change the thinking of critical people -- editorial boards of newspapers, parliamentarians, and so on -- about this issue to complement these 10,000 physicians or health care workers who will be out there with improved skills.
The Chairman: How will you train 10,000 physicians for $1 million? That is only $100 per physician.
Dr. Singer: That is a very good question, and one with which we have struggled. We started with 12,000 and I bargained them down to 10,000.
We plan to use a distributive model. Even though the donation was to the University of Toronto, we plan to build a national partnership of health educators across the country, like the people you heard from before. You heard them say that their problem was funding for their educational programs, et cetera. We want to bring together people geographically as well as by specialty, develop the curricular materials, locate the educational influentials and serve as, if you will, a clearing house to keep track of these physicians. It is a distributive model of education and very consistent with cutting-edge principles of continuing education.
None of us will do the front-line work. We will join in partnership with our colleagues across the country to do this. This system is already in place in continuing education through the colleges. Recently, the colleges have required continuing education on the part of health care workers, both family physicians and specialists. We want to target some of those requirements to end-of-life care. If we were going to do it along a conferencing format and had a vision that we would do it ourselves, there is absolutely no way that we could do it. However, if we can use this $1 million to leverage work with our many dedicated colleagues across the country and work with the colleges and so on, then we can do it. Moreover, it is based on cutting-edge principles of continuing education, which say do not go show someone a lecture but give them the materials and set up the interactive groups of 10 physicians across the country. We want to provide the educational infrastructure for that, not necessarily employ the teachers to do it because there are already dedicated teachers with the skills to do it, as you have heard from many others in other testimony.
It is a challenge. We want to make this a transformative program. We know from continuing education research that you have to get a particular proportion of the whole workforce -- 57,000 physicians in the country -- to achieve a transformative and sustainable change. That is why we aimed at 10,000.
The Chairman: Even if you just get them all talking about it, it will be a positive achievement.
Dr. Singer: No, not at all. What you must realize is that we are talking about something different from training specialists. Let me take a step back.
Some 220,000 Canadians die in the country each year. About one quarter of them die from cancer; three quarters die from something else. Palliative care services are primarily targeted in the cancer model. They are dealing with one quarter of the people who die. I am not arguing they should be, I am just arguing that that is often how they are set up for historical reasons. Of the one quarter of the people who die of cancer, generously, let us say, one half have access to palliative care expertise. You are looking at an overall penetration rate of 12.5 per cent in terms of access to specialized palliative care services. You ought to fund more, and you ought to recommend funding more.
The fact is that most of those people who die will be treated by people like me. We want to bring up the level of skills of people like me one notch. Thus, it is not an in-depth two-year training of a specialist. It is 10 to 12 hours targeted on critical cases and critical issues in the right educational format on the part of 10,000 people and then setting them up in a network where they can continue to learn from each other. Using e-mail list serves, Web sites and so on will have a great effect on how the other proportion of people who die in the country receive their care because they receive that care from people like me.
The Chairman: Dr. Chochinov, you have been engaged in five to eight years of research relating the effects of depression on attitudes of people who are dying. I know that you have contact with all of the physicians and with the palliative care centres in our hometown of Winnipeg. Are they now treating for depression?
Dr. Chochinov: Depression is now being recognized as a clinical entity that accounts for some suffering that we see among the dying.
There was a recent survey of psychopharmaceutical intervention in patients at the end of life, and the prevalence rates of patients who are receiving treatment is still lower than prevalence rates of depression appeared to be, so we are only making initial headway.
The paper that I cited from the Annals of Internal Medicine is another example of how research can heighten sensitivity on the part of care providers to being able to recognize depression.
Many of the studies that have been done thus far have looked at trying to determine what is the extent of the problem. What is lacking in the area of research, and what very much needs to be moved into, is the whole area of interventional research. At this point in time, there are no randomized, controlled trials of anti-depressants among the terminally ill. There are a few smaller trials that have shown them to be efficacious, but a good, randomized, controlled trial is yet to be done. We still have a long way to go in doing the proper intervention trials.
That is probably true in palliative care in general. The focus in the literature has been to try to define the scope of the problem, whether in terms of symptom management or the extent of existential suffering, and so on. What is lacking is research into the domain of interventions.
The Chairman: Senator Roche was not there, but Senator Corbin, Senator Beaudoin and myself were in Winnipeg when Dr. Chochinov first presented in September 1995. I had just joined the committee. When he came with his, at that point, preliminary research data, my immediate reaction was: "Of course they are depressed. They are dying." It seemed quite an obvious statement. However, what you are now telling us now is that it is still not obvious to a lot of people that these people might be depressed.
Dr. Chochinov: The fact is that it is a significant minority of patients who suffer from depressive syndrome. We make the distinction between clinical depression, or depressive syndrome, and the kind of sadness that all of us, of course, experience in the face of life's adversities.
Senator Roche: Dr. Chochinov, you made it clear that you want the committee to concentrate on palliative care and to get off assisted suicide and euthanasia. I thought your presentation was fascinating, and I congratulate you for it, but it was a little fast so I am having trouble recalling precisely what you said. If I am not mistaken, you did introduce euthanasia and assisted suicide. I would ask you to take me through it again. Does the knowledge that you are going to die, and a subsequent depression over it, increase the desire for assisted suicide or euthanasia, or did I get that wrong?
Dr. Chochinov: There is an association between clinical depression and those who would disavow their prognosis. There is also a very direct correlation between those who are clinically depressed and those who may desire a hastened death. One of the studies that I presented indicated that, if you are in that group of patients who have a genuine desire or express a genuine desire for life to be over sooner, the chance of your being depressed is probably 10 to 12 times greater than if you do not have a desire for death.
Senator Roche: If one has a desire for death, it does not mean that that person is seeking assisted suicide or euthanasia.
Dr. Chochinov: That is correct. Senators may be interested in an article in this week's issue of the New England Journal of Medicine. There are three interesting studies that you may wish to look at. One of them looked at complication rates in assisted suicide and euthanasia in Holland and found that the complication rate is in the order of about 20 per cent. The other two studies, which are particularly important, report on the experience in Oregon following passage of their Death with Dignity Act. As senators know, that act passed with a 60 per cent majority. In other words, of every 10,000 Oregonians, 6,000 indicated that the Death with Dignity Act -- assisted suicide -- would be good social policy. The articles in this week's New England Journal of Medicine said that, of those 10,000 Oregonians, if you now move them forward to time of their death, only 60 actually made a request for a lethal prescription. Of those 60, only 10 were deemed to fall within the guidelines of the Death with Dignity Act, and of those 10, five, in fact, died of a lethal overdose. While 60 per cent of Oregonians may support this as good social policy, only one half of a tenth of a per cent actually availed themselves of that policy.
Senator Roche: That is very interesting, and I hope the research staff will look at the material that has been referred to.
I will try to sharpen the question. I did not quite get it out a minute ago. Just because you have a desire for death, it does not mean that you are seeking assisted suicide and euthanasia, and you have confirmed that, but it might.
What I am concerned about here is the public perception and, again, the governmental response.
I know, Senator Carstairs, we are probably going to have this discussion later on when we consider the manner in which the report is going to touch on this subject. Just because we are dealing with palliative care and all the questions associated with palliative care in this study, which I endorse, I have yet to quite understand how we are going to separate ourselves totally from euthanasia and assisted suicide questions that are in the public mind and with which so much of the public identifies palliative care. Maybe I just have not finished sorting it all out in my own head, but I will try the following question on you.
I put it to you that it is impossible to totally separate these questions. Just because we want to deal in this report with palliative care questions, the evidence you have given leads me to believe that I do not see how we can ignore saying something about it, even making the point that palliative care is not assisted suicide. However, when you get to the desire for death, how can we avoid dealing with the question?
Dr. Chochinov: I think you do so just by saying upfront that you are not going to deal with the questions of changing social policy and that you are going to understand desire for death as being one of those indicators of suffering among patients who are nearing death.
Senator Roche: You mean we should go upfront in our report?
Dr. Chochinov: Absolutely. After you have changed the title, the preface would stipulate that although there are many social policy issues to be considered that is not the focus of this study. This study will broach issues like euthanasia, assisted suicide, and desire for death, and will understand those issues as expressions of suffering among the dying.
Senator Roche: I put it to you that the more people understand the virtues and values of good palliative care, the less public desire there will be for assisted suicide.
Senator Beaudoin: That is what I think.
The Chairman: I do not think that either of the witnesses would disagree with that. Dr. Chochinov, let us say that we are writing the report and want to make a reference to some of the research that you have done. Would you be content with a comment to the effect that your research would indicate that one of the issues that must be dealt with in good palliative care is the issue of depression among patients at the end of their life?
Dr. Chochinov: Absolutely, but I think that you need to go broader than that and talk about the whole area of symptom control and symptom management. However, in terms of depression, it absolutely needs to be included.
Senator Corbin: In terms of the research, is near-death depression a particularity of western culture? Let me expand. I have had discussions with persons of other cultures and, from what I have heard, it seems to be that depression is not for them necessarily an end-of-life issue or problem at all.
Has your research been cross-cultural, or have you targeted one group of persons to the exclusion of others? How do you resolve issues such as these, because Canada is very much a multicultural, multi-religious, multi-ethnic country. What credibility can I give your research if I place it in that context?
Dr. Chochinov: Each time I present my research, someone will always ask me: Have you taken this or that fact into account? The answer is that the research is limited. There are only so many factors that can be taken into account, both because of the limitation of the researchers to anticipate them all and because of the expertise of the researchers to incorporate all of those things into a palliative care protocol.
Also, this is a difficult population to study. If you start to include issues such as culture, ethnicity and religion, it expands the length and, thus, the burden of the protocol that is being administered to patients.
Most of the research we have done has taken place in one of Winnipeg's two in-patient palliative care facilities. There is a broad spectrum of cultures represented within those communities, but, again, primarily an older, cancer population.
Earlier on I was asked why we primarily studied cancer patients. The reality is that the majority of patients who enter palliative care facilities have cancer.
Your comments are well taken, in that we cannot necessarily generalize to all ages, cultures and groups. Nevertheless, it is my hope that they shed some light on an area that has essentially lived in darkness for much of the time.
Senator Beaudoin: In the report, we have made a lexicon. I believe it is very well done, but I am open for discussion if there is a mistake. I do not see one at this moment. However, I never close the door; I like discussion.
In my opinion, and this is where there is a problem in this country and all over the world, people disagree on some definitions. Some people do not even see a difference between refusal of treatment and euthanasia. I disagree strongly with them. However, I am ready to hear them.
The title of the lexicon looks very vague, but I agree with Madam Chair -- let us for get about it and we will deal with that in due course.
I congratulated those who moved for the formation of this committee because of their foresight. However, it seems that people do not want to follow through on the issues to which we had previously agreed. In all areas on which we agreed, palliative care, withdrawal of services, and so forth, why do we not proceed?
The title of this report would be very easy to find, but I do not want to freeze everything right at the beginning. However, we must convert people and assure them that there are some distinctions. Philosophy in law is the basis of this subject matter. However, we need a definition. We need a lexicon. We need to discuss the issue.
At the end, we agree or disagree. It will always be like that on this beautiful planet. Do you agree that this is what we should do?
Dr. Singer: Yes, I do agree. However, I wish to push that further. You might consider making three moves in your report. First, I would address the issue of euthanasia and assisted suicide versus the other matters. When you say, people confuse it, really what they are saying is that they think it should be legal or illegal, and you want to put that aside up front.
There are, by the way, some things you can point to, like guidelines from the Chief Coroner's Office of Ontario, that clearly distinguish at the level of action, analgesia and sedation, which is palliative care, on the one hand from euthanasia and assisted suicide on the other.
Your second move is to take together these disparate ideas -- palliative care, advanced directives, life-sustaining treatment -- and put them into a unifying process upon which people can focus. I spent five years of my life studying advanced directives before I figured out they were a little piece of the puzzle, an important piece of the puzzle; but that little piece of paper would not do the trick. I stepped back in order to determine the conceptual nub of this problem. You may wish to consider pulling these things together as an issue of quality end-of-life care.
The third step you ought to consider is not just increasing understanding, but thinking about some concrete strategies for improvement.
Senator Beaudoin: Improvement of what?
Dr. Singer: Improvement of quality end-of-life care.
Senator Beaudoin: Nobody wants to die.
Dr. Singer: No, but what they particularly do not want, senator, is to die in pain, short of breath, hooked up to a machine, alone. Nobody wants to die, but what they especially do not want is that public vision. That is why most people say that quality end-of-life care in Canada rates about a "C".
You can still have the same 222,000 deaths in a year, but move from that "C" to an "A". That is what I think the committee ought to strive towards.
In addition to pulling it together as a single concept, you need to move beyond understanding to some improvement strategies, linked closely to the idea of organizational and health systems' accountability and performance. Those are the things that will ultimately drive the system towards quality end-of-life care, in addition to the things we have done already in palliative care, at the clinical level and at education. Something new is needed. These are some innovations that will drive us in that direction.
Senator Beaudoin: You say something new is needed. We have definitions on refusal, withdrawing, withholding, sedation, palliative care -- perhaps I missed some; I apologize if I did. We do not have to improve that. It is clear-cut.
Dr. Singer: I agree. However, my point is that I practice at the bedside. If I am trying to teach a group of medical students or residents how to approach a dying patient who is in front of us, I can talk about advanced directives, I can talk about life-sustaining treatments, I can talk about pain, but those are little pieces of the puzzle. They still do not have a comprehensive way to think about it, like they have a comprehensive way to think about heart failure.
What we need to do is step back and ask what our goal is here. Our goal is to ensure that the patient in front of us receives quality end-of-life care. How do we do that? Every day we go to the bedside and ask: Are the pain and symptoms controlled? Have we had the discussions we need about life-sustaining treatments? Have we done what we can to support the patient and family? That may seem simplistic to you, but that is an example at the bedside level of an organized conceptual framework.
In my remarks, I have taken that same big-picture view to the level of health care institutions and have framed it as an issue of accountability and thought about how to start to measure it and improve it. It ties very well to my friend Dr. Chochinov's recommendations. In the annual report that he spoke about, what is it that you should have? You should have measures of how Canadian health care systems are performing on this important parameter called quality end-of-life care. Take that organized approach that we developed at the bedside and move it up to the organizational and health systems level in terms of recommendations that we can make in that regard. If I go to the bedside, I talk to the resident or the medical student about a little piece of the puzzle at a time. It will be hard for them to move forward, because they do not see the big picture. The big picture is quality end-of-life care. The third level you have go to is to think about some improvement strategies for that target.
Dr. Chochinov: Many of the discussions talked about the hurdles and difficulties euthanasia and assisted suicide euthanasia create in this discussion and about that being an impediment to moving the agenda forward. There are two others that we have not discussed. The first is, perhaps, a lack of political will. Unfortunately, in end-of-life care, we do not have a vocal constituency. The dead are no longer here to speak, the dying often cannot speak, and the bereaved are often too overcome by their loss to speak. That is a problem.
The second issue is something that we touched on in some earlier testimony, namely, the issue of funding and funding for research. Research funding is necessary to generate knowledge, and knowledge defines the ceiling. The level of care can only rise as high as that ceiling. Let there be no confusion. There was some discussion wherein we were told there was not enough funding and then later on that, perhaps, there was enough funding. I will be the tie-breaker: There is insufficient funding for end-of-life care research.
I was involved in a project funded by Health Canada to create a national palliative care research agenda. I would be happy to submit the findings of that report. It used an external consultation report that looked at each of the major funding agencies in terms of the amounts of funds that are available. MRC, which has a global operating budget of $200 million annually, could identify six grants in the last five years, only one of which was funded at the level of $39,000. The National Cancer Institute of Canada did somewhat better. Of the moneys that they have given out in the last five years, $500,000 was given to end-of-life care projects, which represents about .03 per cent of their operating budget. In this overview, it appears that Health Canada has funded about 25 projects, to the tune of about $7 million. Looking over the list of those projects, most of them are educational initiatives and synthesis and dissemination projects.
Fundamental research needs to be done to generate the knowledge that will be disseminated. The gentleman from NHRDP indicated that $1.2 million over the last five years has been spent on palliative care research. He provided me with a list of those projects. Approximately $400,000 is related to synthesis projects, $400,000 to support two career scientists, and the remainder for a smattering of small projects.
Let there be no confusion about the issue: We are woefully lacking funds. In preparing my comments for today, I spoke to a senior palliative care researcher this past week. That individual, who is considered one of Canada's pre-eminent researchers, indicated that there is uncertainly whether, in a year from now, there will be jobs. Frankly, it be would easier to be a research assistant working in someone else's lab than to deal with the frustrations of trying to find ongoing sustained support.
Senator Roche: What is the percentage of existing palliative care that is occupied by cancer patients?
Dr. Singer: I was going from the 222,000 people who die to say that about one quarter of them die from cancer. Most of the palliative care is focused in the cancer domain. Let us assume that half the people who die of cancer have access to palliative care.
Senator Roche: Is that an assumption?
Dr. Singer: Yes, these are assumptions.
Senator Roche: You are assuming that 50 per cent of people who die from cancer have access to palliative care?
Dr. Singer: That is a complete guess.
Senator Roche: Your friend is not agreeing with you.
Dr. Chochinov: With all due respect, I think the answer is probably considerably lower. The importance of your point is still salient.
Dr. Singer: If it is one quarter, then it is 6.75 per cent. You must think of the following from a population-based perspective: Annually, about 222,000 people die. You want access to palliative care for many of them, and funding for that should be increased for the ideal circumstances that you were hearing about in the previous circumstance. However, you will never get to the point of 100 per cent access for palliative care special expertise, and maybe you should not. Less than 100 per cent of people with heart failure are cared for by cardiologists. A lot of them are cared for by general internists such as myself. My point goes back to the integration issue.
Senator Roche: Are you making the point that more than the cancer patients who are dying require palliative care?
Dr. Singer: Yes.
Senator Roche: In other words, cancer patients get a head start into palliative care. Is that right?
Dr. Singer: Yes. Palliative care grew up, historically, from the Dame Cicely Saunders Hospice in the U.K. It grew up in the cancer model. The main point I am making is that it deals with one quarter of the deaths.
Senator Roche: You say that palliative care includes but goes far beyond cancer?
Dr. Singer: Yes, and in two ways. First, you want organized palliative care specialist services not only for the quarter of people with cancer but also for all deaths <#0107> that is, other than the 10 per cent of people who have sudden deaths.
Second, you do not want to think about dealing with this access issue only as an issue of increased specialist services; rather, you also want to build the skills of front-line doctors and nurses who are caring for those 222,000 people who die, their own core competencies in end of life. I am coming back to the issue that was raised earlier, namely, that every practising physician or nurse who deals with dying people, while not a palliative care expert specialist certified by their college, should have the same level of core skills in end-of-life care as they do in treating people with health care or any other problem.
The Chairman: Thank you very much. It has been very informative. We will have to shut the cameras off now. I need the permanent members of the committee to stay. We must approve our budget for this coming session. I should like everyone to leave except those people required for our next discussion.
Honourable senators, we have a budget to approve. As you can see, the amount is very small -- namely, $7,890. Item 2 is video conferencing. That item would be to update the information, because our second mandate was to update information that was in the other report. At this point, I am not sure we necessarily want to use that process. We may want to use the researchers.
My first recommendation is that we get the information from the researchers about what has happened in the Netherlands, Australia and Oregon. If we then feel it is necessary, we can do a video conference with one, two or three of those countries. However, I want it in the budget so that we will have the money if in fact we agree to proceed that way.
Senator Corbin: That is a reasonable approach.
Senator Beaudoin: I do not object to that because there is some flexibility here. However, it is difficult to agree with Oregon because it is only one state. Why not England or another country?
The Chairman: Because the others have not moved into this area. In our original report, we looked at all other countries that had a policy with respect to euthanasia and assisted suicide. You will remember our video conference with representatives from the Netherlands.
Senator Beaudoin: Yes.
The Chairman: At that point, they were the only ones; there was no others. The only jurisdictions that have changed between 1995 and now are Northern Territory in Australia, the State of Oregon, and the Netherlands, which has introduced legislation, although it is not yet passed.
Senator Beaudoin: What happened in Oregon?
The Chairman: They have had legislation in Oregon since 1995.
My recommendation is that we allow our researchers to get us the information. If we are content with the information they have given us and we it becomes unnecessary to proceed with video conferencing, then we will not have a video conference; we will simply use that information to update our report.
My concern is the concern that was expressed by the last two witnesses. I do not want us to get off focus at all. I want our focus to be quality death in Canada and not the issue of euthanasia and assisted suicide.
If someone will move that, I can present it to Internal Economy.
Senator Beaudoin: How many members are we?
The Chairman: There are three of a total of five here today.
Senator Beaudoin: I may move it. I have no objection.
Senator Corbin: I am thinking. Northern Territory of Australia, the Netherlands and Oregon allow euthanasia, so what is the point of discussing that issue with them?
The Chairman: We have not made a decision about whether we intend to, but one of our mandates is to update the information of the 1995 report.
Senator Corbin: Even the Netherlands did not contribute much in terms of what we are reviewing, the palliative care context. We were more interested in finding out about their euthanasia policy and approaches. Therefore, I do not believe a discussion with them would be relevant. In fact, I do not see why we would bother talking to Oregon at all.
The Chairman: We are not making that decision today.
Senator Beaudoin: I would not object at all to asking for $5,000 for video conferences. I find that quite reasonable. I am inclined to agree that the choice may not be too good, as we will not hear very much from them.
Can we simply ask for $5,000?
The Chairman: In other words, do not mention the countries?
Senator Beaudoin: Yes.
The Chairman: I do not see why not. That is not a problem. We could eliminate mention of the countries. Then we will have it in the budget and we can decide which countries we wish to have a video conference with.
We will eliminate reference to the countries and simply say "video conferencing". Before we do any video conferencing, we will have an in camera meeting about that.
Is that agreeable?
Senator Corbin: I would much rather get the research staff going on that area, which is our sector of interest at this time. If we talk to Oregon, we would have to talk to New York State, which rejected euthanasia, for all sorts of considerations.
Senator Corbin: I move adoption.
The Chairman: It has been moved and passed.
The subcommittee adjourned.